Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.1 Bogotá Jan./Mar. 2019
https://doi.org/10.22516/25007440.353
Original articles
Barriers to Health Care for Gastric Cancer Patients in Santander, Colombia: Exploratory Stage
1Directora del Registro Poblacional de Cáncer del Área Metropolitana de Bucaramanga. Bucaramanga, Colombia
2Magíster en Salud Pública, Docente cátedra Universidad Industrial de Santander. Bucaramanga, Colombia
3Médico general Universidad Autónoma de Bucaramanga. Bucaramanga, Colombia
Introduction:
Gastric cancer is a public health problem that ranks fifth in world incidence and third in mortality.
Objective:
The aim of the exploratory stage of this study was to describe the barriers to health care perceived by adults with gastric cancer, their caregivers, and their attending physicians in the department of Santander, Colombia in 2015 and 2016.
Methodology:
This is a qualitative study using process techniques and grounded theory analysis based on semi-structured interviews that were codified and categorized with N-VIVO 10.
Results:
Thirteen categories and 182 codes described along 6 axes emerged. The first axis is related to the meaning of cancer and its barriers. The second is related to the primary barriers to health care which are, in order from most frequent to least frequent: administrative, economic, cultural, knowledge, communication and institutional. The third axis consists of strategies to overcome barriers. The fourth consists of strategies to diminish barriers. The fifth is related to feelings and the role of the family, and the sixth contains the patient’s needs.
Conclusion:
Fragmentation and segmentation of the health care system imposes barriers that limit early diagnosis of gastric cancer and timely management. In addition, they threaten the quality of life of the sick adult and her or his family.
Keywords: Gastric neoplasm; gastric cancer; health services; inequities; health system
Introducción:
el cáncer gástrico es un problema de salud pública; ocupa el quinto y tercer lugar en incidencia y mortalidad mundial, respectivamente.
Objetivo:
describir las barreras para la atención en salud percibidas por el adulto con cáncer gástrico, su cuidador y el médico tratante en el departamento de Santander, Colombia-etapa exploratoria en el período 2015-2016.
Metodología:
estudio cualitativo utilizando algunas técnicas del proceso de análisis de la teoría fundamentada a partir de la aplicación de entrevistas semiestructuradas que fueron codificadas y categorizadas con el software N-VIVO 10.
Resultados:
Emergieron 13 categorías, 182 códigos descritos en 6 ejes: el primero relacionado con el significado del cáncer y sus barreras; el segundo con las principales barreras para la atención en salud, cuyo orden de mayor a menor frecuencia fue: administrativas, económicas, culturales, de conocimiento, de comunicación e institucionales; el tercero es las estrategias para superar las barreras; el cuarto, las estrategias para disminuirlas; el quinto, sentimientos y el rol de la familia; y el sexto, necesidades del paciente.
Conclusión:
la fragmentación y segmentación del sistema de salud impone barreras que limitan el diagnóstico temprano del cáncer gástrico y su manejo oportuno. Además, amenazan la calidad de vida del adulto enfermo y su familia.
Palabras clave: Neoplasia gástrica; cáncer gástrico; servicios de salud; inequidades; sistema de salud
Gastric cancer (GC) is a malignancy that is associated with helicobacter pylori infections and with genetic, environmental, occupational and dietary factors. 1-7 Globally, GC is the third cause of mortality and is fifth in incidence with 70% of all cases in undeveloped countries. 8,9 In Colombia, GC has a male-female ratio of 2:1 and occurs around the seventh and eighth decade of life with an average age of onset of 65 years. 10 Its incidences are 18.9 men/100,000 inhabitants and 9.0 women/100,000 inhabitants, while it has mortality rates of 15.6 men/100,000 inhabitants and 7.8 women/100,000 inhabitants. 8 In Bucaramanga and its metropolitan area, its incidence among men is 22.4, its incidence among women is 10.3, its mortality rate among men is 17.3, and its mortality rate among women is 11.1. 11
Non-specific signs and symptoms for the initial stages in 80% adult cases of GC include nausea, vomiting, regurgitation and abdominal distension while dyspepsia, epigastric or retrosternal pain, involuntary weight loss, anemia and dysphagia are also frequently associated with GC.12,13,14,15
The timing of the diagnosis depends on several factors: the country’s level of development, the patient’s socioeconomic status, and the available medical expertise. In Japan, GC screening programs allow early diagnosis and decreased mortality, but developing countries have poor adherence to, and participation in, GC screening. 16-19 Also, adults with low socioeconomic status self-medicate, do not consult physicians in a timely fashion, are diagnosed late and have lower survival rates than do people of higher socioeconomic status. 20 Medical expertise influences diagnosis, timely treatment and 5-year survival rates. Thirty-six percent of all GC patients have three or more primary care consultations before being diagnosed through upper digestive tract endoscopy (EVDA) and biopsies, and prognoses depend on patients’ general conditions, ages, clinical staging and tumor location. 14 In Colombia, gastrointestinal symptoms persist for more than 6 months before diagnosis suggesting lack of knowledge about the need to seek medical attention, as well as low accessibility to specialized care which are barriers to care in the General Social Security Health System (Sistema General de Seguridad Social en Salud - SGSSS). 17
The objective of this qualitative study objective is to describe barriers to health care perceived by adults with GC, their caregivers and treating physicians in the department of Santander, Colombia. It has been funded by grant number 124165741298 of the Administrative Department of Science, Technology and Innovation (Departamento Administrativo de Ciencia, Tecnología e Innovación - Colciencias). This purpose of this study has been to learn about the current situation and problems of oncological patients in specifically in the department of Santander in Colombia where the incidence and prevalence of GC is greater than elsewhere in the country. This article presents results obtained in the exploratory stage of the investigation.
MethodologyThis study’s qualitative methodology is based on the interpretation and organization of the data proposed by the grounded theory of Strauss and Corbin. 21,22 The exploratory stage consisted of semi-structured interviews of 9 participants through which health care barriers became evident. In addition, this stage was used to gain familiarity with the interview, verify the clarity of the questions, and check data interaction.
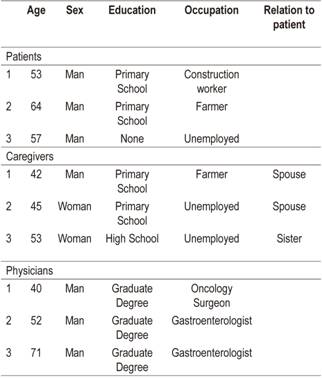
ParticipantsConvenience sampling with emphasis on the quality of the research subjects rather than the number of participants was used. We took into account the perceptions of those who interact directly during health care from the realities in which they live and the roles that they assume during illness. We included three patients (P) from the Cancer Population Registry of the Metropolitan Area of Bucaramanga, Santander who had been, diagnosed with GC between January and March 2015; three caregivers (C) and three doctors (M) (two gastroenterologists and one oncology surgeon). All participants reside in the department of Santander. In total there were seven men and two women with an average age of 53 years (standard deviation of 10.1 years) (Table 1).
Questionnaires and Scripts
There were two types of interviews (I): one consisting of 17 questions for doctors and another of 27 questions for adults with GC and their caregivers. The scripts used by interviewers followed a structure that began with a preamble which was followed by a page of sociodemographic variables and six thematic axes corresponding to the specific objectives set: information about cancer, perceptions and needs, signs and symptoms prior to the diagnosis of cancer, diagnosis and treatment of cancer, barriers to care, and the responses to those barriers.
ProcedureThe treating physician and/or the Health Services Provider Institution (Institución Prestadora de Servicios de Salud - IPS) were called by telephone to contact the sick adult and her or his caregiver. The objectives of the study were explained to them and a guarantee of confidentiality and anonymous handling of interview information was provided. After acceptance, the place, date and time of the interview were agreed upon. During the interview, the participant could opt not to answer any question. Interviewers requested authorization to record the interview. Upon approval, they proceeded to sign the informed consent form and interview the participant according to the script. The interviews were conducted person-to-person by a psychologist in compliance with the recommendation of the Ethics Committee of the Universidad Autónoma de Bucaramanga (UNAB) to maintain a fluent conversation and crisis management in case of presenting. Interviews lasted an average of 40 minutes.
AnalysisThe interviews were transcribed and analyzed using the data coding and categorization system proposed in Strauss and Corbin’s grounded theory method. N-Vivo 10 version 11 was used for description and conceptual ordering without theorization since this was the exploratory stage.
Qualities and characteristics of the data were identified, and participants who shared a common characteristic were grouped together under a name or code derived from precoding or from the inductive subjectivity of the researcher. Subsequently, each code was analyzed and compared to the other codes to identify commonalities to establish relationships between the codes in order to group them into the emerging categories. 22
ResultsEmerging categories are described along the following six axes: perceptions of the words cancer and barrier; barriers to health care; strategies to overcome barriers; strategies to reduce barriers; and feelings, the role of the family, and the patient’s needs.
The meaning of cancer was related to death, handicaps, intimidation, malignity and the design of God. The meaning of barrier was related to obstacles.
The second axis is made up of six barriers to health care. Administrative barriers were oriented to perception of responses obtained during provision of health care for signs and symptoms. These included long term treatments of symptoms without follow-up and absence of exams and procedures. During an interview, one participant (EM) said,
“They usually prescribe something for gastritis, do not do any endoscopy and do not ask for any exam. I think that the main factor is that the patient is treated based on the symptoms and general signs without study.”
During diagnosis, administrative barriers arose including delays of authorization for examinations and procedures, especially upper endoscopy and other procedures requiring attention of a specialist. This generates feelings of dissatisfaction and abandonment among patients. For physicians, administrative problems are obstacles imposed by the SGSSS against medical orders using criteria based on prioritizing health spending on quality of life. As another person (EP) stated in an interview,
“They abandon you ... the EPS (Empresa Promotora de Servicios de Salud - Health Promoter Service, similar to an HMO in the USA) took such a long time that I could have died. The only thing they know is how to charge, they made me run in circles, so I do not feel good about that.”
During treatment, administrative barriers are the result of institutional fragmentation of the SGSSS. This includes problems with procedures to authorize medical appointments and procedures, and in some cases, insurers deny payment, effectively denying treatment unless individuals pay for the appointment or procedure themselves. This reveals the absence of state monitoring of the contracts and institutions that serve adults with GC. As one participant (EM) commented in an interview,
“People get tired of queuing up. In addition, the appointment is given within two months, so people who came from out of town must return home feeling they have wasted the trip.”
Economic barriers are related to the ability of people to cover secondary costs of the disease. For those interviewed, poverty limits their ability to pay these costs and out-of-pocket spending for health care needs and transportation to appointments becomes a source of impoverishment. In some cases, work absenteeism pressures patients to stop treatment.
Cultural barriers are evident in participants answers regarding the search for alternative and/or naturopathic medicine, use of over-the-counter drugs and advice from pharmacists, and word of mouth referrals. As the same participant (EM) said,
“A poor farmer must make his own decisions even if they are wrong, like going to alternative medicine, where they say they can cure everything.”
Knowledge barriers identified include difficulties of general practitioners to associate signs and nonspecific symptoms or their persistence with GC. These include vomiting, burning, stinging, weight loss and gastritis. Also, primary care tends to begin and end with treatment of symptoms, although occasionally a patient is referred to a gastroenterologist. As the same participant (EM) said,
“A doctor does not need to be a scientist but should be a person with an integral concept in health who must know the semiological foundations of the disease, have good judgment and reason and know the epidemiology of gastric cancer.” EM.
Communication barriers are flaws in the doctor-patient relationship attributable to lack of belief and trust on the part of patients and their families in the language, information and explanation provided by health care professional. This influences their understanding and acceptance of the disease. As the same participant (EM) said,
“100% of my cancer patients know. I tell everyone everything. Depending on their cultural level, I use the most comfortable way to explain to them that they have a serious illness.”
Institutional barriers include the excessive time prior to award of medical appointments that lead patients and family to adopt strategies such as begging and insistence. One result is that appointments are not prioritized by the complexity of the clinical picture. Participants perceive that the duration of the health care process between onset of symptoms and diagnosis can be 12 to 18 months, and the time between diagnosis and the start of treatment can vary between one and six 6 months.
In addition, the ways to overcome barriers identified by physicians are education, comprehensive care (inter-institutional medical meetings) and admission of patients admission to the emergency department. For patients, their strategies are religious beliefs and faith in God whereas caregivers face the task of getting money to meet pressing needs.
To reduce barriers to health care access, it is necessary to create medical centers that specialize in oncology and which are supported by the State so that they can direct enough resources to guarantee the health care process and eliminate the endless and counterproductive red tape.
On the one hand, depending on a patient’s perception of his or her condition, one of the strongest consequences can be the inability to continue working and diminution of capacity to earn income and consequent failure to satisfy needs. Similarly, patients feel that EPSs fail to protect them, but they highlight the importance of family for providing moral and financial support as well as for providing basic health care.
On the other hand, doctor and caregivers perceive needs for education for patients and caregivers directed towards motivating and directing health care. Patients and caregivers see needs for timely and comprehensive medical attention, financial support, and help from insurers to pay for shelter and home health care.
DiscussionThis study has found that barriers to health care perceived by the participating adults with GC, their caregivers and treating physicians are either due to the condition of the individual or are secondary to the structure of the SGSSS. The identification of these barriers allows correlation with impacts on mortality and quality of life of the population of the Metropolitan Area of Bucaramanga that influence the prognosis of GC because they sharpen feelings of stress and anxiety, reduce patient quality of life, and potentially affect patient survival. 23
The barriers to medical care in countries other than Colombia have been classified into 4 components: acceptability, accessibility, contact and availability. These are similar to the findings of this study. For example, acceptability according to Adauy et al. is related to fear or shame of derived from going to a health care service, distrust of health care professionals and the treatments they prescribe, 24 and to beliefs and myths that influence patients’ perceptions and responses to cancer. In Colombia, medical attention depends on the health care regime to which a patient is affiliated. There are three regimes: the special regime covers 15.7% of the population, the contributory regime covers 21.1%, and the subsidized regime covers 30.6%. The uninsured account for 57.75% of the population. In response, patients self-medicate guided by relatives and pharmacists. Improvement is transient, and diagnosis is late. 25-28 A study of 428 adults with cancer reported that 89.7% had acquired medications without medical prescription due to lack of time to see a doctor, delays in the health care system, and difficulties of access related to their place of residence. 29 Faced with these barriers, the response of patients and caregivers is to use non-traditional medicine and home remedies. 26,30-33
This is associated with barriers to accessibility caused by excessive waiting times due to Colombia’s fragmented health care system mediated by authorization procedures for medical appointments and procedures that are sometimes denied due failures to hire health care personnel by health service providers, often because of failure of insurers to pay. 24,30,34 All of this limits patient follow-up, as evidenced in our interviews. This in turn creates the perception among patients and caregivers that the SGSSS’ response capacity is poor, and this results in increased out-of-pocket expenses. (25,29,35
ConclusionIdentification of barriers to health care for GC has generated strategies aimed at overcoming those barriers. Moreover, this study shows that the orientation of health services needs to change towards integral attention that exceeds the market logic of the system and which favors patient-centered operations of the SGSSS that take the social environment and its social determinants into account since the most frequent barriers were of administrative origin secondary to institutional segmentation and operational fragmentation of the SGSSS. This would reduce health care time and increase the survival time and rates for adults with GC.
LimitationsThis study could not quantify impacts of the barriers for GC health care on mortality and survival because of its methodology. Additional studies that would correlate barriers for GC health care with patient survival in Bucaramanga and its metropolitan area have been suggested.
Acknowledgements
We thank Colciencias for its support of this study
REFERENCES
1. Torre LA, Siegel RL, Ward EM, Jemal A. Global Cancer Incidence and Mortality Rates and Trends--An Update. Cancer Epidemiol Biomarkers Prev. 2016;25(1):16-27. doi: 10.1158/1055-9965.EPI-15-0578. [ Links ]
2. Goral V. Etiopathogenesis of Gastric Cancer. Asian Pac J Cancer Prev. 2016;17(6):2745-50. [ Links ]
3. McColl KE. Clinical practice. Helicobacter pylori infection. N Engl J Med. 2010;362(17):1597-604. doi: 10.1056/NEJMcp1001110. [ Links ]
4. Raei N, Behrouz B, Zahri S, Latifi-Navid S. Helicobacter pylori Infection and Dietary Factors Act Synergistically to Promote Gastric Cancer. Asian Pac J Cancer Prev. 2016;17(3):917-21. [ Links ]
5. Massarrat S, Stolte M. Development of gastric cancer and its prevention. Arch Iran Med. 2014;17(7):514-20. doi: 0141707/AIM.0013. [ Links ]
6. Jayalekshmi PA, Hassani S, Nandakumar A, Koriyama C, Sebastian P, Akiba S. Gastric cancer risk in relation to tobacco use and alcohol drinking in Kerala, India--Karunagappally cohort study. World J Gastroenterol. 2015;21(44):12676-85. doi: 10.3748/wjg.v21.i44.12676. [ Links ]
7. Wen XY. Salt taste sensitivity, physical activity and gastric cancer. Asian Pac J Cancer Prev. 2010;11(6):1473-7. [ Links ]
8. World Health Organization. International Agency for Research on Cancer. GLOBOCAN; 2012: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012. Population Fact Sheets. GLOBOCAN [internet] 2012 [acceso el 10 de octubre de 2016]. Disponible en: Disponible en: http://globocan.iarc.fr/Pages/fact_sheets_population.aspx . [ Links ]
9. Chang Y, Cho B, Son KY, Shin DW, Shin H, Yang HK, et al. Determinants of gastric cancer screening attendance in Korea: a multi-level analysis. BMC Cancer. 2015;15:336. doi: 10.1186/s12885-015-1328-4. [ Links ]
10. Blanco O, Cantillo A, Rivera J. Enfoque actual del cáncer gástrico. Medicas UIS. 2013;26(2):59-70. [ Links ]
11. Uribe C, Osma S, Herrera V. Cancer incidence and mortality in the Bucaramanga metropolitan area, 2003-2007. Colomb Médica. 2012;43(4):290-7. [ Links ]
12. García C. Actualización del diagnóstico y tratamiento del cáncer gástrico. Rev Méd Clin Condes. 2013;24(4):627-36. [ Links ]
13. Gómez MA, Riveros JH, Ruiz O, Concha A, Betamcur DMA, Torres M, et al. Guía de práctica clínica para la prevención, diagnóstico y tratamiento del cáncer gástrico temprano - 2015. Rev Colomb Cancerol. 2015;30(1):34-42. [ Links ]
14. Astin MP, Martins T, Welton N, Neal RD, Rose PW, Hamilton W. Diagnostic value of symptoms of oesophagogastric cancers in primary care: a systematic review and meta-analysis. Br J Gen Pract. 2015;65(639):e677-91. doi: 10.3399/bjgp15X686941. [ Links ]
15. Mayer RJ. Upper gastrointestinal tract cancers. En: Kasper D, Fauci A, Hauser S, Longo D, Jameson J, Loscalzo J (editores). Harrison’s Principles of Internal Medicine. 19.a edición. Nueva York: McGraw-Hill; 2014. p. 447-60. [ Links ]
16. Calvo A. Diagnóstico precoz del cáncer gástrico: estrategias de prevención secundaria y dificultades del diagnóstico de lesiones precoces. Rev Méd Clin Condes. 2011;22(4):477-84. [ Links ]
17. Oliveros R, Navarrera LF. Diagnóstico, estadificación y tratamiento del cáncer gástrico en Colombia desde 2004 a 2008 (REGATE-Colombia). Rev Colomb Gastroenterol. 2012;27(4):269-74. [ Links ]
18. Lee KJ, Inoue M, Otani T, Iwasaki M, Sasazuki S, Tsugane S; et al. Gastric cancer screening and subsequent risk of gastric cancer: a large-scale population-based cohort study, with a 13-year follow-up in Japan. Int J Cancer. 2006;118(9):2315-21. doi: 10.1002/ijc.21664. [ Links ]
19. Higashi T, Machii R, Aoki A, Hamashima C, Saito H. Evaluation and revision of checklists for screening facilities and municipal governmental programs for gastric cancer and colorectal cancer screening in Japan. Jpn J Clin Oncol. 2010;40(11):1021-30. doi: 10.1093/jjco/hyq091. [ Links ]
20. Siemerink EJ, Hospers GA, Mulder NH, Siesling S, van der Aa MA. Disparities in survival of stomach cancer among different socioeconomic groups in North-East Netherlands. Cancer Epidemiol. 2011;35(5):413-6. doi: 10.1016/j.canep.2011.02.015. [ Links ]
21. Noerager P, Jane C. Essential of accesible grounded theory. 1.a edición. Estados Unidos: Left Coast Press; 2011. p. 42. [ Links ]
22. Strauss A, Corbin J. Bases de la investigación cualitativa, técnicas y procedimientos para desarrollar la teoría fundamentada. 1.a edición. Colombia: Editorial Universidad de Antioquia; 2002. p. 11-28. [ Links ]
23. Hamlyn GS, Hutchins KE, Johnston AL, Thomas RT, Tian J, Kamal AH. Accessibility and Barriers to Oncology Appointments at 40 National Cancer Institute-Designated Comprehensive Cancer Centers: Results of a Mystery Shopper Project. J Oncol Pract. 2016;12(10):e884-e900. doi: 10.1200/JOP.2016.014159. [ Links ]
24. Adauy M, Poffald L, Jasmen AM, Aguilera X, Delgado I, Vega J. Barreras y facilitadores de acceso a la atención de la salud: una revisión sistemática cualitativa. Rev Panam Salud Pública. 2013;33(3):223-9. [ Links ]
25. Garcia-Subirats I, Vargas I, Mogollón-Pérez AS, De Paepe P, da Silva MR, Unger JP, et al. Barriers in access to healthcare in countries with different health systems. A cross-sectional study in municipalities of central Colombia and north-eastern Brazil. Soc Sci Med. 2014;106:204-13. doi: 10.1016/j.socscimed.2014.01.054. [ Links ]
26. Kagawa-Singer M, Dadia AV, Yu MC, Surbone A. Cancer, culture, and health disparities: time to chart a new course? CA Cancer J Clin. 2010;60(1):12-39. doi: 10.3322/caac.20051. [ Links ]
27. Pinzón CE, Ospina J. Dispepsia: un real desafío diagnóstico. Rev Cienc Salud Bogotá. 2008;6(1):50-70. [ Links ]
28. Galindo F. Carcinoma gástrico. Cirugía digestiva. 2009;II-223:1-31. [ Links ]
29. Del Toro M, Díaz A, Barrios Z, Castillo IY. Automedicación y creencias en torno a su práctica en Cartagena, Colombia. Rev Cuid. 2017;8(1):1509-18. [ Links ]
30. Restrepo JH, Silva C, Andrade F, Vh R. Acceso a servicios de salud: Análisis de barreras y estrategias en el caso de Medellín, Colombia. Rev Gerenc y Polit Salud. 2014;13(27):242-65. doi: 10.11144/Javeriana.rgyps13-27.assa. [ Links ]
31. Hernández A, Vega R. El sistema colombiano de seguridad social en salud: desigualdad y exclusión. Rev Gerenc y Políticas Salud. 2001;1(1):48-73. [ Links ]
32. Hunt R, Quigley E, Abbas Z, Eliakim A, Emmanuel A, Goh KL, et al. Manejo de los síntomas gastrointestinales frecuentes en la comunidad. Perspectiva mundial sobre acidez, estreñimiento, distensión y dolor o molestia abdominal. Guías Mundiales de la Organización Mundial de Gastroenterología; 2013. [ Links ]
33. Woods LM, Rachet B, Coleman MP. Origins of socio-economic inequalities in cancer survival: a review. Ann Oncol. 2006;17(1):5-19. doi: 10.1093/annonc/mdj007. [ Links ]
34. Garcés IC, Rubio DC, Ramos SM. Barreras y facilitadores del sistema de salud relacionadas con el seguimiento de anormalidades citológicas, Medellín-Colombia. Rev Gerenc y Polit Salud. 2014;13(27):200-11. doi: 10.11144/Javeriana.rgyps13-27.bfss. [ Links ]
35. Vargas I, Vázquez ML, Mogollón AS. Acceso a la atención en salud en Colombia. Rev Salud Pública. 2010;12(5):701-12. doi: 10.1590/S0124-00642010000500001. [ Links ]
Received: June 12, 2018; Accepted: October 02, 2018











 text in
text in