Introducción
Endoscopic guided biliary stent placement is a procedure used in patients with stenosis of the biliopancreatic confluent secondary to unresectable neoplasias, and ERCP is the technique of choice to perform such procedure 1. Even being the method of choice, ERCP fails in 5% to 10% of cases 2 due to situations such as anatomical alterations, gastroduodenal obstruction, obstructed segment of considerable length, distortion of the papilla, periampullary diverticulum, and duodenal stents 2. Traditionally, if ERCP fails, percutaneous transhepatic cholangiography is performed, a procedure in which complication and morbidity rates can be up to 33% 2, including catheter dysfunction and associated cholangitis, bile leak or bleeding to the peritoneal cavity. In case of failure with the two abovementioned techniques, surgery is the final treatment option; however, this approach implies the morbidity of undergoing any surgical intervention. For these reasons, endoscopic ultrasound (EUS)-guided biliary stent placement has emerged as a drainage alternative.
The clinical case of a female older adult with a biliary obstruction secondary to a malignancy who underwent an EUS-guided metal stent placement after undergoing a failed biliary stent placement using ERCP is presented.
CASE DESCRIPTION
This is the case of a 72-year-old female patient with a biliary obstruction secondary to a mass located in the head of the pancreas. The following findings were reported in her paraclinical tests: laboratory tests: initial total bilirubin levels of 12.32 mg/dL at the expense of direct bilirubin levels (10.8 mg/dL); abdominal CT scan: presence of a neoplasm in the head of the pancreas surrounding in 180° the superior mesenteric vein; patent splenoportal confluence; patent hepatic artery; dilatation of the intrahepatic and extrahepatic biliary ducts, and of the main pancreatic duct; increased density of mesenteric fat with lymph nodes with short axes (between 5 mm and 6 mm) suspicious due to their enhancement; and focal hepatic lesion in the segment 6 with an appearance suggestive of suspected neoplastic infiltration, without presence of free fluid (Figures 1 and 2).
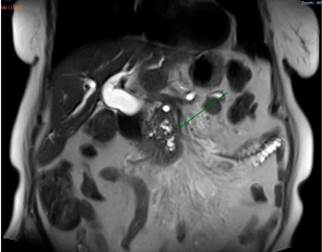
An abdominal MRI showed a dilatation of the intrahepatic and extrahepatic biliary ducts associated with a mass located in the head of the pancreas, with signs of involvement of the root of the mesentery and the presence of a focal hepatic lesion in the sixth segment of suspicious appearance (Figure 3).
Based on these findings, palliative care was decided by performing a biliary stent placement by means of an ERCP. During the procedure, the papilla was found to be distorted with local retraction of the duodenal walls, and despite cannulation of the distal bile duct was achieved, cannulation of the proximal bile duct was unsuccessful. EUS-guided biliodigestive shunt was then performed, in which a neoplastic infiltration of the duodenal papilla preventing its cannulation and a 23 mm heterogeneous hypoechoic lesion in the head of the pancreas with an up to 18 mm retrograde bile duct dilation were found (Figure 4). An initial puncture of the mass was performed for histological study purposes and then of the transduodenal bile duct with a 19 Fr. needle, which allowed the advancement of the 0.035” hydrophilic guide wire; dilatation was achieved using a biliary balloon dilator under fluoroscopic control and subsequent placement of the 10 x 80 mm fully covered metal stent was performed, which was released under endoscopic and fluoroscopic control achieving adequate opening and drainage of the contrast medium and clear bile, without subsequent complications (Figures 5 and 6). The cytology report of the samples obtained through endosonography confirmed adenocarcinoma involvement. Two months later, a total bilirubin control was performed obtaining the following results: total bilirubin: 2.42 mg/dL; direct bilirubin: 1.85 mg/dL, and indirect bilirubin: 0.58 mg/dL (Figure 7). Palliative care was continued in the oncology service.

Figure 5 Endoscopic-guided bile duct cannulation and fluoroscopy in which dilatation with distal amputation is observed.
Discussion
This is the case of a patient with an obstruction of the distal common bile duct secondary to an inoperable adenocarcinoma located in the head of the pancreas, who required undergoing biliary stent placement due to the effects of compression. In this regard, similar cases describing the inability to cannulate the biliary duct due to the compressive nature of malignant tumors have been documented, but this situation has also been described in obstructions caused by benign tumors3-6.
EUS-guided biliodigestive shunt is an alternative procedure when failure to access the papilla or the bile duct occurs using ERCP (5% to 10% of cases)7; when the failure is caused by anatomical alteration, as it happened in the case presented here; or when ampullary distortion, periampullary diverticula, gastric outlet obstruction or in situ duodenal stents are present2.
When ERCP fails, biliary stent placement is then performed using percutaneous transhepatic cholangiography, but adverse events occur in up to 33% of cases, including hemorrhage, bilioperitoneum, infection and acute cholangitis, among others8. On the contrary, EUS-guided biliodigestive shunt has a lower risk of adverse events.
Transhepatic drainage is associated with significant morbidity. There are reports of complications in up to 60% of biliodigestive shunts performed using transpariticohepatic cholangiography, compared to 35% of those performed using EUS3.
EUS-guided biliodigestive shunt was first described by Giovannini et al. in 20019, and its safety and efficacy are currently being demonstrated given its approach2; in addition, it offers the following advantages: it is a minimally invasive procedure, it can be performed immediately after a failed ERCP and by the same specialist, it allows the drainage of both intrahepatic and extrahepatic bile ducts, it is a procedure that only causes mild pain to the patient (and even it does not cause any pain at all in some cases), it does not involve external drainage or dislocating the drains, it does not restrict the patient’s ability to engage in their daily activities as it only requires a very short hospitalization time, and it has a low complication rate3,10,11.
Regarding its complications, a 3.4 % to 38.6 % complication rate with an average complication rate between 17 % and 18.9 % has been described3,12,13; however, the rate of complications has shown a decreasing trend over time10,13-15. Complications include bile leak (3 %), hemorrhage (2.7 %), cholangitis (0.3 %), sepsis and peritonitis (3.5 %)10. Serious complications include the migration of the stent into the peritoneal cavity and fatal perforations, but their frequency is very low10,16,17; however, a consensus regarding the complications of this procedure has not yet been defined2.
As mentioned before, the performance of biliodigestive shunts through percutaneous transhepatic cholangiography is associated with a lower clinical success rare and, therefore, a higher cost. ERCP and EUS have the same efficacy to perform a biledigestive shunt, but there are no prospective studies comparing EUS as a primary procedure to perform biliodigestive shunts2.
Cannulation of the papilla can be quite complex in cases where the obstruction is caused by a malignant tumor, and, therefore, cannulation time increases, which can trigger the development of adverse events, being post-ERCP pancreatitis the main adverse event, which can occur in up to 10% of cases in which cannulation time exceeds 10 minutes18.
In this sense, the last multi-institutional consensus determined that EUS-guided biliodigestive shunt is the technique of choice in patients with a bile duct obstruction secondary a malignancy and in which bile stent placement was not possible using ERCP. In this regard, the following management algorithm has been proposed (Figure 8)1.
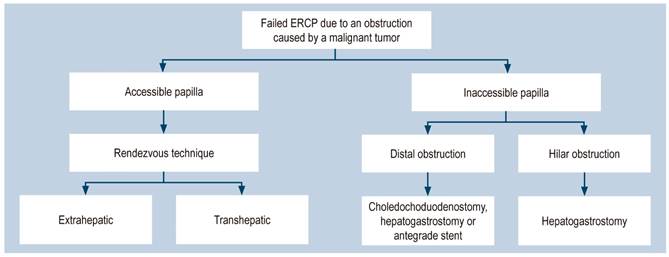
Figure 8 Management algorithm for patients with failed ERCP due to an obstruction caused by a malignancy1. Taken from: Guo J et al. Endosc Ultrasound. 2018;7(6):356-365.
It has been demonstrated that this is a safe and effective procedure for the management of obstructions secondary to malignant tumors with very similar results when compared to ERCP. In fact, it can be thought that it is not only the method of choice in cases of failed ERCP, but also in distal intestinal obstruction cases. In addition, due to the fact that it is performed under direct observation, the risk of acute pancreatitis can be avoided.
Conclusion
EUS-guided biliodigestive shunt is an emerging technique that is considered a very good alternative in patients in which initial ERCP was unsuccessful. It is a practical, effective and efficient procedure with an adequate safety margin and clinical response. As it is an emerging technique, further studies are required to consolidate such advantages.











 text in
text in