Introduction
The sphincter of Oddi, first described by Ruggero Oddi in 18871, is a system of sphincters composed of connective tissue, circular and longitudinal smooth muscle fibers mostly found within the duodenal wall. The system is composed of three sphincters: the sphincter of the common bile duct, the pancreatic sphincter and a common sphincter where the muscle fibers of the other two sphincters intertwine in an 8 shape way2.
The sphincter of Oddi is responsible for regulating the flow of bile and the exocrine secretion of the pancreas; it prevents the reflux of enteric contents from the duodenum into the pancreatic and biliary system, and it diverts bile into the gallbladder between meals, which facilitates its physiological concentration. During fasting, the sphincter of Oddi maintains pressures ranging from 3 mm Hg to 35 mm Hg (a pressure > 40 mm Hg is considered to be abnormal), with contractions that promote the flow into the duodenum, with an average frequency of 4 contractions per minute with an average duration of 6 seconds. Although there is a relationship with the migrating motor complex of the duodenum, most of the bile flow seems to be passive between the contractions of the sphincter of Oddi and increase due to gallbladder contraction, antral distention, the effect of cholecystokinin, and a decreased amplitude of the contractions of the sphincter in the postprandial state3.
Sphincter of Oddi dysfunction is a clinical syndrome caused by a functional (dyskinesia) or a structural (stenosis) disease4. It is clinically characterized by the presence of abdominal pain, similar to biliary colic or pancreatitis-like pain in the absence of an organic biliopancreatic disease. It should also be suspected in patients with recurrent idiopathic acute pancreatitis; pain and pancreatitis must be associated with elevated levels of pancreatic or hepatic enzymes, or with dilatation of the common bile duct or the pancreatic duct5.
This syndrome occurs more frequently in women between 20 and 50-years old who have undergone a cholecystectomy. The estimated prevalence of sphincter of Oddi dysfunction in the general population is 1%, but in patients with persistent postcholecystectomy pain and in those with recurrent idiopathic acute pancreatitis it increases to 20 % and 70%, respectively. However, its true prevalence cannot be easily determined due to the lack of definitive biomarkers or diagnostic criteria6-10.
Risk factors of sphincter of Oddi dysfunction include the presence of choledocholithiasis, cholesterosis, pancreatitis, ascaridiasis and malignancy, and the performance of endoscopic retrograde cholangiopancreatography (ERCP) or the surgical manipulation of the bile duct5.
The Milwaukee classification for sphincter of Oddi dysfunction, which divides patients into 3 types based on its clinical presentation and altered laboratory and imaging findings, is used for its diagnosis (Table 1)11-13. Somehow, the Rome IV classification, which describes 2 types of biliary sphincter of Oddi dysfunction and one third type corresponding to episodic functional abdominal pain, was published in 2016 (Table 2)14.
Table 1 Milwaukee classification for sphincter of Oddi dysfunction15.
ALT: alanine aminotransferase; AST: aspartate aminotransferase; ALP: alkaline phosphatase. Taken from: Madura JA 2nd et al. Surg Clin North Am. 2007;87(6):1417-29, ix.
Table 2 Criteria for the diagnosis of both biliary and pancreatic sphincter of Oddi dysfunction (ROMA IV classification)14.
To the best of our knowledge, to date, in Colombia there are no case reports describing a sphincter of Oddi dysfunction case; moreover, there is controversy regarding the diagnosis and treatment of this condition.
Clinical case
This is the case of a 67-year-old woman who received treatment for cholelithiasis in another health institution and who underwent a laparoscopic cholecystectomy in 2013; besides, she had a history of dyslipidemia which was being treated with atorvastatin. After the surgical procedure, she repeatedly visited the emergency department due to abdominal colicky pain predominantly located in the right hypochondrium, together with bile vomiting; however, normal liver function tests values were found in all these episodes. In December 2016, a magnetic resonance cholangiopancreatography (MRCP) showed the surgical absence of the gallbladder, a dilatation of the intrahepatic bile duct in the left lobe with an 8 mm common bile duct, and absence of choledocholithiasis (Figure 1). Normal values were reported in both the complete blood count test and the liver function tests (Table 3).

Figure 1 MRCP. Postcholecystectomy status, dilatation of the intrahepatic bile duct in the left lobe, common bile duct of 8 mm.
Table 3 Postcholecystectomy laboratory tests results
| Laboratory test | Results |
|---|---|
| Complete blood count |
|
| Liver function tests |
|
In October 2017, she was evaluated in a medical consultation by our service, where, due to her clinical signs and her surgical history, sphincter of Oddi dysfunction was suspected. A hepatobiliary iminodiacetic acid (HIDA) scan was then requested. The HIDA scan was performed in November 2017 and the following findings were reported: “elimination to the intrahepatic duct before 15 minutes with abundant retention in the major hepatic ducts and the common bile duct. A score of 9 points was obtained in the Sostre scale for sphincter of Oddi dysfunction (scores > 5 points are consistent)” (Table 4,Figure 2).
Table 4 Sostre scale score.
| Oddi’s dysfunction. Sostre Score | Points | Patient |
|---|---|---|
|
|
|
1 |
|
|
|
1 |
|
|
|
1 |
|
|
|
2 |
|
|
|
1 |
|
|
|
3 |
| Total | 9 |
A score of 9 points was obtained in the Sostre scale for sphincter of Oddi dysfunction (scores > 5 points are consistent).
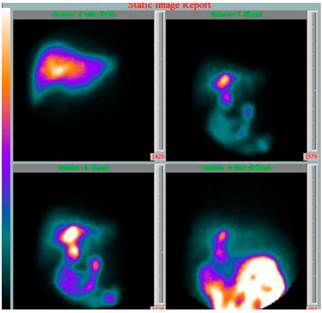
Figure 2 HIDA scan, elimination to the intrahepatic duct before 15 minutes with abundant retention in the major hepatic ducts and the common bile duct.
Based on these findings, a type II sphincter of Oddi dysfunction diagnosis was considered and an ERCP plus a biliary endoscopic sphincterotomy were performed in February 2018, in which a normal major papilla and dilated intra- and extrahepatic bile ducts were documented (1.3 cm). The biliary endoscopic sphincterotomy was carried out and the bile duct was explored with a basket up to the hepatic duct, obtaining a clear biliary fluid outflow.
After performing the ERCP, the patient’s condition improved satisfactorily and there were no complications. In February 2020 (2 years after the ERCP), date in which the patient attended her last follow-up visit, she was asymptomatic and normal values were reported in her complete blood count test. In addition, the patient did not visit the emergency department anymore after the ERCP was performed.
Discussion
We present the case of a patient in which a postcholescytectomy sphincter of Oddi dysfunction diagnosis was suspected. Since diagnosis was supported by the HIDA scan findings, an ERCP was performed achieving a complete resolution of the patient’s symptoms and clinical signs.
Clinically, differentiating sphincter of Oddi dysfunction from other biliopancreatic diseases, as well as from other functional digestive tract disorders is not an easy task. However, the medical record and physical examination, laboratory and imaging findings must be carefully evaluated in order to suspect its diagnosis.
The referral of patients with this condition to health centers with expertise in the treatment of biliopancreatic diseases is fundamental for their outcome, where laboratory tests (hepatic and pancreatic enzymes) and imaging studies, including abdominal ultrasound, abdominal tomography, MRCP, biliopancreatic endosonography (EUS) or isotopic techniques such as hepatobiliary scintigraphy, must be requested prior to the assessment of the patient’s symptoms10.
Regarding the analysis of the sphincter of Oddi dysfunction diagnosis, it can be noted that in patients with bile duct dilatation, diagnosis is suspected based on the symptomatology and complete blood count results; when there is a high probability of biliary disease and other causes have been ruled out based on previous imaging findings, performing an ERCP is suggested16. On the contrary, in the case of bile duct dilatation, but low probability of biliary disease (symptomatology and complete blood count results), performing an EUS or a MRCP is suggested, since the diagnostic performance of these procedures is similar to that of ERCP, but they don’t have the morbidity and mortality associated with the latter16. Specifically, in the context of bile duct assessment, EUS has a diagnostic performance of only 53 % in patients with bile duct dilatation and abnormal complete blood count results16, which decreases to 6% in patients with bile duct dilatation and normal complete blood count results16. This 6% is associated with factors such as age over 65 years and having undergone a cholecystectomy16.
The use of ERCP plus sphincter of Oddi manometry have been recommended for studying sphincter of Oddi dysfunction. In patients with clinical suspicion of the condition and any objective alteration associated with a biliary disease (type II sphincter of Oddi dysfunction), an elevated sphincter of Oddi pressure (> 40 mm Hg) while in resting position is a diagnostic criterion for sphincter of Oddi dysfunction, as well as a good predictor of symptom resolution after undergoing a biliary endoscopic sphincterotomy. However, the probability of developing post-ERCP pancreatitis and sphincter of Oddi manometry pancreatitis can be up to 30 %11,17-19. In our opinion, this level of risk associated with the performance of a diagnostic study is unacceptable, not to mention the fact that the possibility of false negatives can be up to 65%20,21.
Research has been conducted on diagnostic and therapeutic methods including Nardi test, secretin-enhanced MRCP, cholecystokinin scintigraphy, functional luminal imaging probe, calcium channel blockers, tricyclic antidepressants, nitroglycerin, somatostatin and botulinum toxin. To date, none of the above alternatives has been shown to have relevant clinical usefulness22-29.
Biliary endoscopic sphincterotomy is indicated in patients with type I sphincter of Oddi dysfunction; no other additional studies are required in these patients20,30. On the contrary, in those with type II and III sphincter of Oddi dysfunction, diagnosis and management are controversial. In our opinion, a hepatobiliary scintigraphy should be performed before ERCP in all patients with suspected type II and III sphincter of Oddi dysfunction, provided that this nuclear medicine procedure has, at least, a specificity of 90%14,31-34. In addition, in the evaluation of postcholecystectomy biliary colic-like pain, scintigraphy is included in the diagnostic algorithm14.
Treatment in patients with type II sphincter of Oddi dysfunction consists of biliary endoscopic sphincterotomy, because clinical response, despite being variable, is generally favorable when the procedure is performed by an expert, with some reports describing that this treatment is successful in up to 90% of cases. We do not suggest performing a sphincter of Oddi manometry prior to the biliary endoscopic sphincterotomy because of the aforementioned risks of complications and the debatable relationship between sphincter of Oddi manometry findings and sphincter of Oddi dysfunction12,35-37.
Patients with type III sphincter of Oddi dysfunction are the most difficult to diagnose due to the absence of abnormal laboratory and imaging finings; in addition, there is controversy regarding their treatment. These patient do not benefit from the performance of ERCP and biliary endoscopic sphincterotomy (the severity of symptoms decrease only in approximately 20%)38-41; on the contrary, they are exposed to the risks inherent to these procedures42. Therefore, treatment in these patients must be symptomatic and based on medications used to treat functional gastrointestinal disorders43.
In conclusion, we suggest suspecting sphincter of Oddi dysfunction in patients who present with symptomatology compatible with biliary colic-like pain or pain of pancreatic origin after having undergone a cholecystectomy; likewise, the diagnostic suspicion should be based on tools other than sphincter of Oddi manometry (scintigraphy) that, based on their specificity, allow making a decision regarding the performance of an ERCP plus a biliary endoscopic sphincterotomy to achieve the resolution of symptoms.
Finally, this case serves as a starting point for conducting prospective studies in other population groups.











 text in
text in 



