Introduction
The coronavirus disease 2019 (COVID-19) was initially believed to be a respiratory illness, but its potential consequences on other organs, including the digestive system, have become increasingly apparent over time.1 The first confirmed case of COVID-19 with gastrointestinal symptoms was reported in the United States.2 This discovery suggested the possibility of fecal-oral transmission, as the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was detected in stool samples, which drew further attention to the difficulty of assessing virus infectivity and potential alternative modes of transmission.3 Studies conducted outside of China also described a higher incidence of gastrointestinal symptoms,4 including diarrhea, loss of appetite, nausea, vomiting, and abdominal pain. In addition, dysgeusia, anosmia, and gastrointestinal bleeding were reported upon admission or during hospitalization.3
SARS-CoV-2 infection is associated with gastrointestinal involvement and may require diagnostic and therapeutic endoscopic studies for patients with diverse clinical manifestations. The suspicion of intestinal bleeding is a common indication in hospitals, but multiple etiologies must be considered, including the underlying viral disease, medication consumption, coagulation disorders, and ischemic involvement.1 The need for nutritional support also increases the need for endoscopic support.3,5 Prior studies have found abnormal endoscopic findings in a significant proportion of the patients under study, ranging from mild to severe disease severity and displaying considerable heterogeneity in endoscopic findings.5-7 It is reported that gastrointestinal involvement in COVID-19 patients is clinically relevant and that those with gastrointestinal symptoms often experience more severe clinical outcomes and require more intensive treatment.8,9
It had been proposed previously that the gastrointestinal tract could be a potential target of SARS-CoV-2 due to possible direct inflammatory effect on the gastrointestinal mucosa, as the virus binds to angiotensin-converting enzyme 2 (ACE-2) receptors that are constitutively expressed in the gastrointestinal tract.10 However, previous studies5,7,11 have shown heterogeneous findings and determined that most gastrointestinal manifestations are related to critical or prolonged illness rather than direct viral injury. In our setting, there is limited data on the severity of COVID-19 and its potential relationship with gastrointestinal involvement detected by endoscopic studies. Thus, the primary objective of this descriptive study is to report the need for endoscopic procedures in a sample of hospitalized patients with moderate to severe COVID-19, and the secondary objective is to describe the characteristics, findings, and interventions in detail.
Study Design and Data Extraction
A cross-sectional descriptive observational study was conducted from May 2020 to December 2021, in which data from 2312 hospitalized patients who required endoscopic studies were collected from two third-level hospitals in Bogotá, Colombia. The study included patients aged 18 years or older diagnosed with moderate to severe COVID-19 who were hospitalized in the emergency room, general ward, or intensive care unit (ICU) and underwent endoscopic gastrointestinal procedures for any indication during their hospital stay. Subjects with mild COVID-19 and those who underwent endoscopic gastrointestinal procedures as outpatients were excluded.
Data Collection
For data collection, we relied on medical records and official reports of procedures, which served as our primary source of information. We gathered sociodemographic and clinical variables and analyzed information on indications, endoscopic findings, interventions, anesthesia use, and adverse events. The collected variables included age, sex, endoscopic indication, type of endoscopic study conducted, endoscopic findings, requirement for ventilatory support, need for sedation by anesthesiology during the procedure, requirement for hemostasis, and any adverse events encountered.
Definitions
The definition of Moderate COVID-19 in this study was based on clinical evaluation or imaging showing evidence of lower respiratory disease and oxygen saturation (SpO2) ≥ 94% in ambient air. Severe COVID-19 was defined as having a SpO2 < 94% in ambient air, a ratio between arterial partial pressure of oxygen and the inspired fraction of oxygen (PaO2/FiO2) < 300 mm Hg, a respiratory rate (RR) > 30 breaths per minute (brpm), or pulmonary infiltrates > 50%.12 For cases of documented esophagitis, the severity was classified according to endoscopic findings using the Los Angeles classification.13
Statistical Analysis
We utilized MS Excel version 2019 to create the database. Any missing data was completed through further revisions of the sources of information, and only complete data were ultimately analyzed. The data was processed using the social sciences program SPSS version 25.0. Descriptive analysis utilized the arithmetic mean and standard deviation (SD) for quantitative variables, while absolute and relative frequencies were used for qualitative variables.
Ethical Considerations
The Ethics and Research Committees of Clínica Palermo and Clínica Infantil Santa María del Lago in Bogotá, Colombia, approved this study. Both hospitals are third-level care centers and local referral centers in gastroenterology. The study design followed the requirements established in Resolution 8430 of 1993 of Colombia’s Ministry of Health and Social Protection, ensuring confidentiality and discretion with the collected information, and was considered low-risk research. All patients provided informed consent, and no records contained sensitive information about patients’ identities.
Results
During the study period, 2312 patients with moderate to severe COVID-19 were hospitalized in the participating institutions, of which 63 (2.72%) were included in the study and underwent endoscopic procedures. Most of these patients were male (75%) and had an average age of 65.7 years. Of the total, 41 patients (65%) met the criteria for severe COVID-19, while 22 had moderate disease. Upper endoscopy (EGD) was the most common procedure, followed by colonoscopies and endoscopic retrograde cholangiopancreatography (ERCP). The most frequent indications for these procedures were gastrointestinal bleeding (62%), enteral access requirement (28.3%), and cholangitis (4.8%), among others (Table 1).
Table 1 Characterization of patients with moderate-severe COVID-19 requiring endoscopic studies
| Characteristics (n = 63) | |
|---|---|
| Average Age (SD) | 65.73 (13.91) |
| Sex | |
| - Male, n (%) | 47 (75%) |
| - Female, n (%) | 16 (25%) |
| Endoscopic indication | |
| - Bleeding, n (%) | 39 (62%) |
| - Gastrostomy requirement, n (%) | 14 (22%) |
| - Cholangitis, n (%) | 3(4.8%) |
| - Catheter for nutritional support, n (%) | 4 (6.3%) |
| - Abdominal pain, n (%) | 1 (1.6%) |
| - Foreign body, n (%) | 1 (50%) |
| - Intestinal obstruction, n (%) | 1 (50%) |
| Endoscopic study | |
| - EGD, n (%) | 51 (81%) |
| - Colonoscopy, n (%) | 9 (14%) |
| - ERCP, n (%) | 3 (4.8%) |
ERCP: endoscopic retrograde cholangiopancreatography; EGD: upper endoscopy; SD: standard deviation. Source: Authors’ own research.
Out of the 39 patients with suspected digestive bleeding, six (15.38%) required hemostatic therapy (Table 2), and all of them were treated with adrenaline sclerotherapy. The most commonly affected region by ulcers was the stomach, with seven out of nine patients, followed by the duodenum, with two out of nine patients. Ischemic involvement was documented in three patients, of which two had ischemic esophageal involvement (Figure 1), and the other had gastric ischemic involvement. These cases were observed in patients who met the severe COVID-19 definition and required ICU admission due to systemic thrombotic involvement. Gastrostomy was performed in fourteen cases (22%), and four required nasoenteral catheters (6.3%) (Table 1). ERCP was required in three cases, and findings of choledocholithiasis were documented (Table 2).
Table 2 Endoscopic findings of patients with moderate-severe COVID-19 requiring endoscopic studies
| Endoscopic findings (n = 63)* | |
|---|---|
| Erythematous gastritis, n (%) | 14 (22.2%) |
| Esophagitis, n (%) | 10 (15.8%) |
| Ulcer, n (%) | 9 (14.3%) |
| Hemorrhagic pangastritis, n (%) | 6 (9.5%) |
| Changes due to epistaxis, n (%) | 3 (4.8%) |
| Choledocholithiasis, n (%) | 3 (4.8%) |
| Erosive gastritis, n (%) | 3 (4.8%) |
| Diverticular bleeding, n (%) | 2 (3.2%) |
| Erosive bulboduodenitis, n (%) | 2 (3.2%) |
| Ischemic involvement, n (%) | 3 (4.76%) |
| Neoplasm, n (%) | 1 (1.6%) |
| No findings, n (%) | 27 (42.8%) |
*Patients may have more than one endoscopic finding. Source: Authors’ own research.
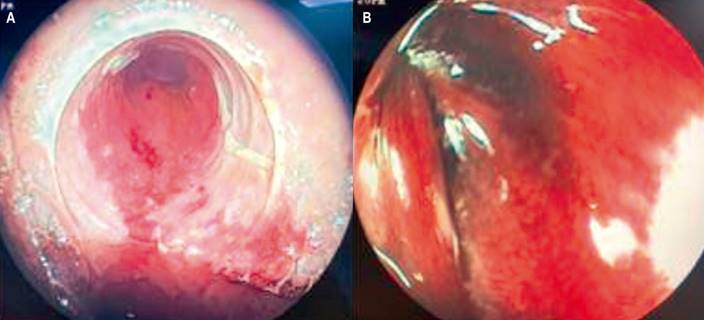
Figure 1 Endoscopic view of ischemic esophageal involvement. A. Detachment of areas of mucosa in an early stage of ischemic esophagitis. B. Advanced involvement in areas of necrosis. Images owned by the authors.
During the endoscopic procedures, 65% (n = 41) of the patients were receiving ventilatory support and sedation. Of those cases, 22 required participation from anesthesiologists for general anesthesia due to their classification of III or higher in the American Society of Anesthesiologists (ASA) and multi-support therapy. No negative pressure room was used during any of the procedures, and no data were collected regarding the possible exposure and infection of endoscopy or anesthesia personnel during these procedures.
Discussion
Despite the high burden of COVID-19, only 2.72% of the 2312 hospitalized patients with moderate to severe COVID-19 required endoscopy. Most EGD findings showed erythematous gastritis and esophagitis, while diverticular bleeding was the most common finding during colonoscopy. Gastrointestinal bleeding was the most common indication for EGD, likely due to interrelated factors such as medication use, predisposition to bleeding, or disseminated intravascular coagulation. We observed cases of esophageal and gastric ischemia, which may be secondary to thrombotic dysfunction resulting from excessive inflammation, platelet activation, and endothelial dysfunction. Findings in the upper gastrointestinal tract are consistent with those of previous studies conducted in Italy and the United States,5,6,14 and are expected in severely ill patients. In contrast, we did not observe any findings of inflammatory pathology in the colon, which is similar to the outcomes of a study by Kuftinec et al.5 Diverticulosis and hemorrhoids were the main colonoscopy findings in that study. Therefore, the indications and endoscopic findings are likely consequences of systemic disease rather than a direct viral lesion, which is consistent with the findings of previous studies.5,7,11
The majority of participants in this study were male and had an average age of around 65. It is worth noting the occurrence of hemorrhagic and ischemic findings, which suggest the presence of complications in patients with moderate-severity COVID-19. Previous studies5-7,11,14 analyzed people aged 60 to 71, primarily male participants (56%-83.3%), with diabetes and hypertension as the main comorbidities and a higher rate of complications with respect to other age groups. Despite the limitations of this study, our findings highlight the importance of considering the male sex and advanced age as potential risk factors for ischemic damage in the gastrointestinal tract due to COVID-19. Further research is needed in this area. The role of the endoscopist is crucial in the comprehensive and multidisciplinary management of these patients.
Among the 63 patients in this study, 39 (62%) required endoscopy due to digestive bleeding, and six of these cases (15.38%) required hemostatic therapy, which was achieved through adrenaline sclerotherapy. Enteral access was only required in four cases (6.35%), and ERCP was necessary in three cases due to biliary obstruction, all of which were associated with choledocholithiasis with cholangitis. Diagnostic endoscopies accounted for most cases (36/63, 57.1%) and did not require interventional treatment. These findings are consistent with those of Kuftinec et al.5 and suggest that conservative (non-endoscopic) treatment may be an appropriate option for most COVID-19 patients. The decision to perform an endoscopic study with possible intervention should be made by experts based on individual patient needs.
Despite the small sample size, we did not identify a significant increase in risk associated with endoscopic intervention or sedation in our patients. However, some studies have indicated a higher risk of sedation-related broncho-aspiration in patients undergoing colonoscopies under sedation compared to those without sedation (0.22% vs. 0.16%).15,16 This is particularly relevant in patients with COVID-19 who have respiratory involvement and changes in mental state. At the time of the endoscopic study, 41 out of 63 patients (65%) were on ventilatory support and sedation, and 22 out of 41 (53.6%) required anesthesiology assistance for the procedure. No adverse events were documented during the peri-procedural period, and no negative pressure rooms were needed. These findings are similar to those of Kuftinec et al.,5 which reported that approximately 50% of their patients required anesthesiology assistance for endoscopic procedures. Most procedures were performed in the ICU or digestive endoscopy unit, and none required a negative pressure room. Thus, the support of anesthesiology is essential to ensure the safety and comfort of clinicians in the peri-procedural management of these patients.
The study has several potential limitations, including a retrospective design and reliance on medical record reviews. Additionally, the study was conducted in only two third-level hospitals in Bogotá, Colombia, and thus, the results may not apply to other geographic locations with different resource availability. Furthermore, the sample size for patients undergoing EGD was small due to the national considerations for endoscopic procedures during the pandemic, which limited procedures to urgent or therapeutic purposes only. Other limitations include the inability to compare COVID-19 patients to those with negative results in the follow-up period and the lack of histological and microbiological analyses due to the endoscopic approach. Despite these limitations, this study sheds light on the wide range of gastrointestinal manifestations of COVID-19 that gastroenterologists and endoscopists should be aware of.
Conclusions
According to the findings of this study, less than 3% of patients with moderate to severe COVID-19 required gastrointestinal endoscopy. In addition, conservative management was generally employed, and there was a low frequency of endoscopic interventions. The indications for the procedures, as well as the endoscopic findings, interventional requirements, and need for anesthesia, were highly variable and consistent with what has been reported in previous literature. Therefore, clinical judgment is crucial in determining the necessity of endoscopies and prioritizing those that are urgent and therapeutic.











 text in
text in 



