Introduction
The epiploic appendages are anatomical structures that arise from peritoneal extensions. From 50 and 100 epiploic appendages originate in two rows (anterior and posterior) parallel to the external surface of the three longitudinal muscle bands of the large intestine.1 As Sand et al. state, the epiploic appendix was first described in 1543 by Vesalius. However, it did not have clinical significance until 1853, when Virchow suggested that the detachment of the epiploic appendages could be the source of intraperitoneal bodies.2 The term epiploic appendagitis (EA) was first described by Lynn in 1956, while the radiological features were defined by Danielson in 1986.3-5 Epiploic appendagitis is a rare cause of acute abdominal pain and misdiagnosis resulting from inflammation, torsion, or infarction of the vascular pedicle of an epiploic appendix.6 It appears as acute abdominal pain, which may be accompanied by fever, nausea, and vomiting, among others. The incidence of EA is 8.8 per million people7 and is misdiagnosed in medical practice due to the lack of pathognomonic clinical features.8 Treatment is usually self-limiting in most cases; however, this pathology can sometimes recidivate.
Case report
This is a 41-year-old female patient who first went to the emergency service on October 14, 2020, after two days of intense pain in the left hemiabdomen of colic type and intensity 8/10 that did not expand to another area. In addition, twelve hours earlier, she reported nausea and general malaise. As part of her history, she manifested having had a transverse segmental cesarean section. At admission, the patient was awake, with vital signs within normal values (blood pressure [BP]: 120/70 mm Hg, respiratory rate [RF]: 20 breaths per minute [rpm], heart rate [HR]: 78 beats per minute [bpm], oxygen saturation [SatO2]: 96% and afebrile). A physical examination of the digestive system revealed a soft, depressible abdomen with diminished hydro-air sounds and palpation pain in the hypochondrium and left flank. Laboratory tests revealed mild anemia (hemoglobin 9.3 g/dL).
The patient underwent an abdominopelvic computed tomography (CT) with contrast material, which evidenced that the liver, pancreas, spleen, and intestinal loops did not have any significant alteration, the stomach was partially distended with preserved walls and with a hypodense image of the oval fat density of 25 mm x 16 mm that contacts the anterior border of the descending colon, which contains inside a hyperdense image (the sign of the central point) compatible with EA (Figures 1, 2 and 3). She started her medical treatment for pain with diclofenac 75 mg intramuscularly every twelve hours, paracetamol 500 mg orally in only one dose, metronidazole 500 mg orally every eight hours, and simethicone (gaseovet) 15 drops every eight hours. She was indicated to have a soft low-fat diet. The patient was discharged after two days on the following medications: paracetamol 500 mg (10 tablets), tramadol 50 mg (4 tablets), metronidazole 500 mg (9 tablets), and metoclopramide 10 mg (9 tablets).

Figura 1 A. Appendagitis, coronal court S/C. B. Appendagitis, coronal court C/C. Source: Authors’ archive.

Figure 2 Hypodense image (circumscribed by a white circle) of fat density, oval, which contains a hyperdense image (the sign of the central point) inside compatible with epiploic appendagitis. Source: Authors’ archive
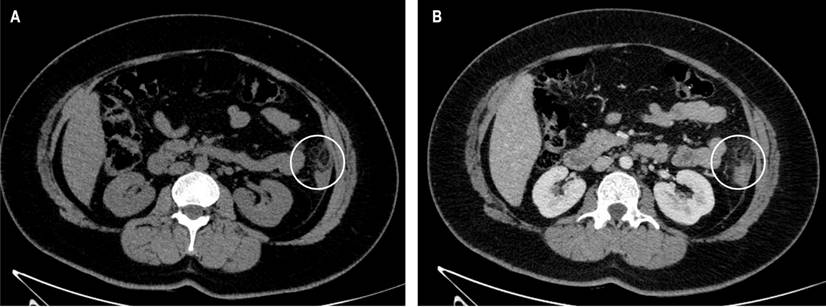
Figure 3 A. Appendagitis, horizontal cut S/C. B. Appendagitis, horizontal cut C/C. Source: Authors’ archive.
Seven months later, the patient went to the emergency department again due to a clinical picture of acute abdomen. Her examinations showed an elevation of leukocytes and neutrophilia. Meanwhile, all other laboratory tests were within normal limits. Abdominopelvic CT showed inflammation of the epiploic appendages in the left colonic framework. She underwent symptomatic treatment with diclofenac 75 mg intramuscularly every 12 hours and paracetamol 500 mg orally once a day.
Discussion
Anatomically, the epiploic appendix is a formation resulting from the duplication of the visceral peritoneum that surrounds the colon and covers a variable amount of pedunculated fat attached by a more or less narrow base to the external surface of the colonic wall. Most appendages are 1 to 2 cm thick and 2 to 5 cm long.6 Inflammation of the epiploic appendix is known as epiploic appendagitis, which occurs due to a twisting of the epiploic appendages that leads to ischemia that subsequently becomes necrosis.9 It is often a misdiagnosed disease that must be present within the differential diagnosis of an acute abdomen, which commonly resembles acute appendicitis, diverticulitis, pelvic inflammatory disease, and ectopic pregnancy, among others.9,10
EA commonly begins with pain in the lower left quadrant (40%-60%), pain in the right lower quadrant (40%-50%), and pain in other locations, including the upper right and left quadrants (1.5%-10%).11 An increase in white blood cells can hardly be found, so the possibility of laboratory aid, including their symptomatological nonspecificity, is dismissed, leading physicians to an incorrect diagnosis. Therefore, the chosen study is CT, and only 2.5% are diagnosed with the symptoms before surgery since normal epiploic appendages are not evident on CT but can be detected when inflamed or delineated by ascites.12 Key features in CT include an ovoid lesion of fat density, also known as the hyperattenuating ring sign, mild thickening of the intestinal wall, and a central focus of high attenuation within the fat lesion that in recent studies has been described as the central point sign.12
EA is usually self-limited following conservative therapy. However, some cases need surgical management. Reports mention that some discharged patients have relapses, forcing them to go to the emergency room again.13 Therefore, we conducted a systematic search in PubMed, Scopus, Scielo, CINAHL, BVS LILACS, Google Scholar, and articles related to the topic in English and Spanish, with the search terms “Epiploic appendagitis” and “Recurrence” or “Relapse”, and we found eleven articles that met the terms of “recaída” and “relapso” in Spanish within the full text, whose characteristics are detailed in Table 1. Only seven patients out of 278 had a recurrence, which means 2.6% relapses. We consider it a small percentage. Relapses are not as common in these patients. However, there are currently minimally invasive techniques, such as laparoscopic surgery, which could help when there is a failure in conservative therapy, or an emergency intervention is needed. In that case, laparoscopic surgery shows better results.14,15
Table 1 Characteristics of included studies of patients with EA
| Author | Country | Type of article | Number of patients included | Sex M/F | Age (SD) | Symptoms/signs | Comorbidities (number of patients) | Diagnosis | Treatment | Recurrence time |
|---|---|---|---|---|---|---|---|---|---|---|
| Choi16 | Korea | Observational, retrospective | 56 | 23/33 | 45.4 (15.1) | Abdominal pain | Obesity (30) | CT | Conservative therapy, antibiotics | One patient recurred five years later. |
| Dogan17 | Turkey | Observational, retrospective | 39 | 34/5 | 36 (10.3) | Abdominal and groinal/low back pain, nausea, vomiting, abdominal swelling, and dysuria | Does not report | CT | Analgesic therapy and antibiotics | No patient in one year of follow-up |
| García18 | Spain | Observational, retrospective | 17 | 3/14 | 57 | Abdominal pain | Does not report | CT | Conservative therapy | One patient had an uncomplicated recurrence. |
| Hasbahceci19 | Turkey | Observational, retrospective | 20 | 13/7 | 43.2 | Acute abdominal pain | Does not report | CT | Conservative therapy | No recurrence at 24 months of follow-up |
| Legome20 | United States | Observational, retrospective | 19 | 10/9 | 37.8 (10.4) | Abdominal pain, constipation (10%), diarrhea (10%), and fever (15%) | Does not report | CT | Antibiotic therapy | One patient recurred at two years of follow-up. |
| Lorente13 | United States | Case report | 1 | 0/1 | 66 | Abdominal pain | Hypertension, hyperlipidemia, hypothyroidism, and cardiomyopathy | CT | Conservative therapy | Recurrence after nineteen months |
| Mantoglu21 | Turkey | Observational, retrospective | 39 | 29/10 | 44.4 (13.2) | Does not report | Does not report | CT | Conservative therapy | One female patient recurred after six months. Two male patients recurred at two and twelve months. 3-year follow-up |
| Ozdemir4 | Turkey | Case series | 12 | 9/3 | 40 | Abdominal pain, nausea, and vomiting | Does not report | Ultrasonography and abdominal CT | Surgical and conservative therapy | Non-recurrence |
| Vázquez22 | Argentina | Observational, retrospective | 73 | 54/19 | 45 (16) | Abdominal pain | Food transgression (7), overweight (26) | Ultrasound, CT scan | Conservative therapy and surgical therapy | Non-recurrence |
| Yang23 | China | Case report | 1 | 1/0 | 44 | Abdominal pain | Does not report | CT scan with contrast | Not treated | Non-recurrence |
| Yousaf24 | Pakistan | Case report | 1 | 1/0 | 26 | Abdominal pain | Does not report | CT | Conservative therapy | Non-recurrence |
SD: standard deviation
Conclusions
Relapses in patients with EA are uncommon. However, more studies are needed to evaluate this outcome in this condition. On the one hand, patients are treated conservatively with analgesics, but there are reports of cases treated surgically that would prevent a recurrence. For this, it is also necessary to evaluate the efficacy of new surgical therapies to resolve this pathology. On the other hand, it is fundamental to keep this pathology in mind within the differential profile of the acute abdomen due to its similarity to various diseases.











 text in
text in 



