Introduction
The first description of a bilioma was made in 1884,1 although the term bilioma was first introduced in 1979.2 It refers to a collection of bile, which may or may not be encapsulated, located outside the biliary tree.3 The most frequent causes include iatrogenesis and trauma.3 The incidence of postoperative bilioma is 0.3%-2%.3,4 The average time from cholecystectomy to the appearance of bilioma is two weeks.5 The incidence of spontaneous or non-traumatic bilioma6 is less frequent and, in adults, is associated with choledocholithiasis.3 It is less frequently associated with hepatic infarction, abscesses, neoplasms, or extrapulmonary tuberculosis.3 Patients may present abdominal pain, bloating, peritonitis, jaundice, and sepsis.3 The average time between the onset of symptoms and diagnosis is between one and two weeks.3,7 Ultrasound, with a sensitivity of 70%,4 and computerized axial tomography, with a diagnostic yield of 90%4, are the most frequently performed imaging studies. The percutaneous ultrasound-guided intervention has diagnostic and therapeutic utility and is recommended as the first line of treatment.2,6 Management of patients may also include antibiotic treatment, especially in cases with sepsis. In cases of asymptomatic collections < 4 cm, only surveillance is performed.3 If percutaneous drainage does not resolve the condition, the patient may undergo endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy and the option of stent insertion.2 Among the differential diagnoses are cysts, seromas, pseudocysts, hematomas, and liver abscesses. On this occasion, we present the case of a patient with spontaneous bilioma.
Presentation of the case
This is a 55-year-old man with a history of laparoscopic cholecystectomy eight years ago. He consulted after two days of abdominal pain in the upper hemiabdomen, more accentuated in the right hypochondrium, colic type, expanding to the back, and associated with fever and nausea.
Laboratory tests at admission found leukocytosis with neutrophilia, hyperbilirubinemia (total bilirubin: 2 mg/dL, direct bilirubin: 1.72 mg/dL), elevated alkaline phosphatase (148 U/L, normal: 35-104 U/L), elevated alanine aminotransferase (ALT: 89 U/L, normal: 0-41 U/L) and elevated C-reactive protein (CRP: 32 mg/dL). He had normal clotting times, electrolytes, azolates, aspartate aminotransferase levels (normal AST: 0-40 U/L), and amylase. Given the suspicion of cholangitis, he started an empirical antibiotic management with ceftriaxone and metronidazole.
The patient underwent an abdominal ultrasound that described dilation of the bile duct with these measurements: the right route (5 mm), the left one (4.8 mm), and the confluence (5.3 mm). A low amount of gas was also described at the level of the intrahepatic bile ducts. He also underwent a magnetic resonance cholangiopancreatography where they found a focal alteration in the subcapsular region of hepatic segment VI with an image of 34 x 31 x 37 mm, of heterogeneous content and similar images of smaller size, 10 and 13 mm, in segment VIII, suspicious of abscesses. Hepatic subcapsular fluid was also documented in the right lobe (112 mL) (Figure 1) and intrahepatic bile duct dilation with images of microlithiasis in the right hepatic duct near the confluence and in the intrapancreatic segment of the common bile duct. After 48 hours, an abdominal MRI was performed, and an increased volume of the hepatic subcapsular collection was found (Figure 2), so the patient was inserted into a multipurpose catheter. In the procedure, 1600 mL of purulent biliary-looking fluid was drained. The patient continued for five days with biliary drainage of 350-500 mL daily through the multipurpose catheter and with signs of an inflammatory response, so he was taken to ERCP.
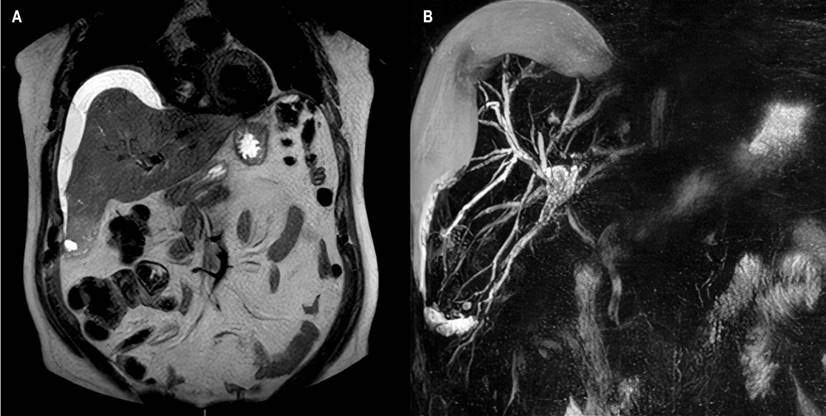
Figure 1 Magnetic resonance cholangiopancreatography. A. In sequence T2, subcapsular collection: bilioma. B. 3D reconstruction of the bile duct. Image Archive of Hospital Universitario Hernando Moncaleano Perdomo in Neiva.

Figure 2 MRI of the abdomen. Increased volume of bilioma is observed. Image Archive of Hospital Universitario Hernando Moncaleano Perdomo in Neiva.
ERCP showed a narrowing of the common bile duct at the junction of the proximal third with the middle third, with dilatation proximal to the confluence of the hepatic ducts (Figure 3A). Papilotmy was performed with drainage of purulent bile fluid and extraction of stones with basket and balloon. It was decided to insert a 10 cm Teflon stent of 10 Fr with adequate drainage (Figure 3B).
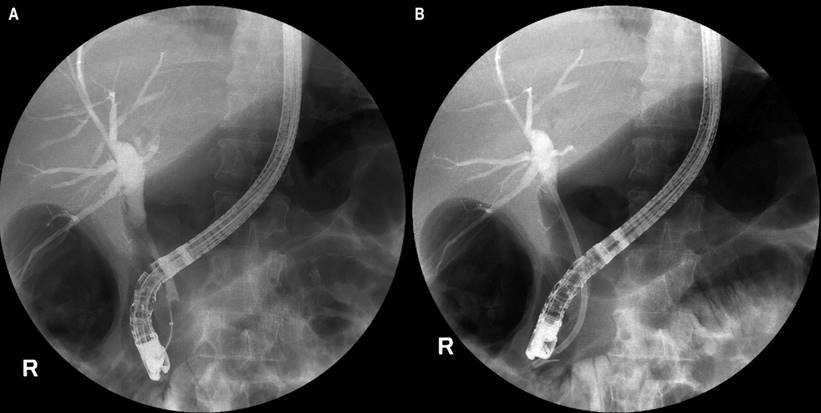
Figure 3 ERCP. A. Dilation of the bile duct at the junction of the proximal third with the middle third of the common bile duct, proximal dilation to the confluence of the hepatic ducts. B. After insertion of 10 Fr Teflon stent of 10 cm. Image Archive of Hospital Universitario Hernando Moncaleano Perdomo in Neiva.
After the procedure, the patient required admission to the intensive care unit (ICU) and invasive mechanical ventilatory support (IMV). Antibiotic treatment was switched to fosfomycin + tigecycline + aztreonam by isolation in the drainage fluid through the carbapenem-resistant multipurpose catheter of Enterobacter cloacae multipurpose catheter by metallobetalactamase.
The patient subsequently presented a favorable evolution, with the tolerance of weaning from IMV the next day and discharge from the ICU. Signs of systemic inflammatory response disappeared on the second day after ERCP. The drainage volume through the catheter was < 50 mL from the third day after the procedure. The catheter was removed on the seventh day after ERCP. A control abdominal ultrasound showed that the residual collection was minimal. The patient was discharged upon completion of seven days of targeted antibiotic treatment with a stent removal plan upon completion of ten weeks.
Discussion
The development of spontaneous bilioma is a rare phenomenon. Cases have been reported in the United States,4,6 Mexico,1 Peru,8 Brazil,3 Serbia,9 Italy,5 and India,2,7 and it is a condition that can occur in both men and women. In these reports, the symptoms presented by the patients include nausea, emesis, the presence of insinuated masses in the abdominal wall, acolia, and choluria,2,3,5,8 in addition to the abdominal pain present in almost all cases.1
Our patient had a history of laparoscopic cholecystectomy for eight years, unlike other reported cases of patients without a pathological or surgical history.2,3 There are case reports of biliomas presented five years,7 nine years,9 and 35 years8 after an open cholecystectomy. Our case is the longest reported time between a laparoscopic cholecystectomy and the appearance of a spontaneous bilioma. The liver profile may be altered in all its parameters, partially altered as in our patient’s case, or not altered at all.2 Our patient presented choledocholithiasis like other cases described,2,3,6 a condition frequently associated with spontaneous bilioma.
In our case, the patient initially underwent an ultrasound, and then, the lesion was better characterized by a magnetic resonance cholangiopancreatography and abdominal resonance. Magnetic resonance imaging has a diagnostic yield of around 95%.4 Our patient required antibiotic treatment due to his septic state, with isolation of a multidrug-resistant germ.
Management included percutaneous drainage, but the patient persisted with abundant drainage and signs of systemic inflammatory response until five days later, so he was taken to ERCP with Teflon stent insertion. In the case of our patient, the increase in bile duct pressure, in addition to the obstruction due to choledocholithiasis proposed as an etiology of these cases of spontaneous bilioma,6 was probably facilitated by stenosis of the common bile duct. For cases that do not resolve with this initial management, ultrasound-guided transmural drainage or transpapillary/transfistular access have been proposed as interventions.10 In one case reviewed, drainage with a T-tube and cholecystectomy were performed after failure of ERCP with sphincterotomy. After the endoscopic intervention, the patient initially had a clinical deterioration but presented a favorable evolution, so he was discharged at the end of the 7-day antibiotic regimen. He could remove the multipurpose catheter due to minimal drainage, with ultrasound evidence of an almost complete reduction of the collection. This is the first case of spontaneous bilioma documented in Colombia.
Conclusion
The occurrence of spontaneous biliomas is an infrequently documented event, possibly because small lesions may be asymptomatic and resolve without specific treatment. In patients with bile duct intervention, this complication should be suspected, and appropriate imaging studies should be used to make the diagnosis early. Most cases resolve with percutaneous drainage, although the endoscopic intervention of the bile duct is necessary for some others.











 text in
text in 



