INTRODUCTION
While many studies have proven a high degree of patients satisfaction with overdentures on implants,(1,2,3) showing that these patients’ quality of life is higher compared to patients with conventional dentures,(4,5) there is also a high number of studies reporting repairs and maintenance of implant-supported dentures.(6,7,8)
Watson et al(9) investigated the need for maintenance and repair of mandibular overdentures, finding out that, in the first year of use, 68% of patients required some type of prosthodontic maintenance.
The repairs and adjustments most commonly required in overdentures fixed with ball attachments include: loss of prosthetic pillar screws, fracture of the ball receptacle, rebasing of the prosthetic base, and ulcerations.(10,11,12)
The high success rate of interforaminal implants used in supporting mandibular overdentures has been well documented, and placing the implants parallel to each other has been recommended, especially when considering individual ball adjustments; another recommendation is to place them on the way of prosthesis insertion, in order to prevent incomplete settlement of the prosthesis and early failure of the adjustments, and to provide an axial load on the implants without causing tensions.(13) Retention can also be maximized by setting implants parallel to each other.(14)
The scientific interest on the forces acting in dental implants that support overdentures has existed for many years. In 1993, Mericske-Stern(15) conducted a study using cephalometric radiographs to observe the relative inclination of implant axis to the mandibular plane of the respective denture. The author found out that 70% of implants showed a buccal inclination, 11% showed a lingual inclination, and only 19% had a 90° angle.
In 2001, Walton, Huizinga and Peck(16) conducted a study aimed at developing a technique to measure the angle between two implants and between each implant to the planes, in order to analyze the relationship between maintenance (adjustments and repair) of ball attachments connecting mandibular overdentures and the angulation of implants.
In 2012, Atashrazm et al(17) conducted a study to evaluate the effect of overdentures on retention and longevity when the implants had an inclination of 5 to 10 degrees.
In 2013, Çeli̇k and Uludağ(18) conducted a photoelastical study to evaluate the effect of implant inclination and the adjustments on load transfer and to compare the different designs of implant-retained mandibular overdentures. As for the model with inclined implants, they observed higher stress patterns in implants retained with a bar, in comparison with certain types of individual non-splinted attachments.
The aim of the present study was to evaluate the sagittal inclination of implants with respect to the occlusal plane of overdentures and their effect on prosthetic behavior after two years of service.
MATERIALS AND METHODS
This was a descriptive cross-sectional study in patients who attended the Clinic of Universidad Autónoma de Manizales Oral Rehabilitation Graduate Program. It involved evaluating the inclination and the clinical and radiographic behavior of 52 implants placed in 26 full mandible edentulous adults who were chosen for rehabilitation treatment with two interforaminal implants (BioHorizons RMR® Biohorizons Internal Implant System) of 3.8 x 15 mm or 3.8 x 12 mm in length, using ball attachments to support the lower overdenture.
The project was endorsed by the Universidad Autónoma de Manizales Ethics Committee (according to Affidavit N.° 12 of 2010). The present study complies with the scientific and ethical principles specified by international standards for health research, described in the Declaration of Helsinki and by the Colombian regulations according to Resolution 8430 of the Ministry of Health of Colombia. This study was classified as a research project with greater risk than the minimum, due to the use of x-rays (exposure to 6 msV per clinical case). Therefore, prior to starting the study, all patients were clearly explained the objectives, risks and benefits of their participation, and only those who signed a written informed consent were included.
Once they accepted, patients were taken lateral head radiographs, in accordance with the standardization of equipment DX-D 300. Tracings were performed on the radiographs based on reference measurements in order to establish skeletal, facial and dental measurements, as well as on the implants; tracings were made on digital radiography through 32-bit OSIRIX® image viewer, version 5.8.2, and Dicom viewer for Macintosh® with the Mac OS operating system, version 10.11.1, prior calibration of the operator.
Tooth position in the maxillary and mandibular dentures was determined by markings with radiopaque resin material on teeth 11 and 31, at the most central point of the buccal gingival surface, the palatal gingival surface and at the center of the incisal edge, so that its radiopacity allowed the tracing on the longitudinal axis, projecting the shaft in an apical direction. For the occlusal plane, the reference point was the area of molars with a resin marking at the tip of the middle buccal cusp of the first left lower molar (LML) buccal cusp and the mesial fossa of the occlusal side of the first left upper molar (UMR); that way, with a maximum intercuspidation, the reference of the occlusal plane of each patient could be obtained.
For the facial or soft tissue assessment, the esthetic line (LE) was taken as reference, tracing the nose point, which corresponds to the outermost point of the tip of the nose and the most anterior and outer point of the chin. There should be 4 mm of distance between the lower lip of the esthetic plane; a higher value would correspond to protrusion and a lower value would be retrusion.
The skeletal relationship was taken based on the tracings of the facial depth angle, which is composed of the Frankfort plane -the horizontal line drawn between Po (porion) and the Or point (orbitale)- and the intersection with the facial plane-the vertical line drawn between point N (nasion) and Pg (pogonion), whose standard is 90° ± 3°-. The three skeletal classes were determined as follows: class I, between 87 and 93°, with the mandible in a harmonic position; class II, retruded position of the mandible with a < 87° value, and class III, protruded position of the mandible, with a > 93° value. Anteroinferior facial height was determined by the angle formed by the ANS (anterior nasal spine) plane and the Xi point (center of the mandibular ramus), and from this point a plane was traced to the point d (center of the mandibular symphysis).
To assess the anteroposterior position or inclination of the implants, the reference was the mandibular plane intersected by the most anterior longitudinal axis of the implant, similar to the tracing of the longitudinal axis of the natural mandible incisor (aIIm: angle of inclination of the implant to the mandibular plane); Similarly, implant inclination was analyzed with respect to the prosthetic occlusal plane (aIIpop: angle of inclination of the implant with respect to the prosthetic occlusal plane), determining the buccal or lingual inclination of the implant.
The angle of compensation of the implant (aCI) was established, which is the inclination that the mandible implant must have in antero-posterior direction for class I occlusal stability. It was determined by tracing the axis of prosthetic compensation (outer-most anterior point of the implant and inclination of the prosthetic incisor) and intersecting it with the longitudinal axis of the implant to obtain the angle of compensation of the implant (Figure 1).

Figure. 1: Cephalometric landmarks: LE: aesthetic line; FH: Frankfort plane (Po: Porion to Or: Orbitale); PF: Facial plane (N: nasion to PG: Pogonion); ENA: anterior nasal spine; XI: point Xi; d: point d (center of symphysis); PM: Mandibular plane (Go: Gonion to Me: Chin); POP: prosthetic occlusal plane; aIIpop: aIIM: angle of inclination of the mandibular implant; aIIpop: angle of inclination of the implant with respect to the prosthetic occlusal plane; aCI: angle of compensation of the implant.
The data were recorded in an Excel® spreadsheet and, after consolidating all data, they were exported to the statistical package SPSS version 21. The analysis was made with measures of central tendency and variability. The qualitative variables were analyzed with absolute and relative frequencies. The bivariate analysis evaluated the sagittal inclination of the implant with respect to variables of clinical and radiographical behavior. The comparison of means was made with the Student’s t test, and correlations were tested with the Pearson correlation coefficient, taking the p-value < 0.05 as statistically significant.
RESULTS
A total of 26 patients were evaluated, 70.4% of which were females and 29.6% were males. The average age was 67.93 ± 8.6 years. The follow up period ranged from 23 to 33 months, with an average of 29.85 ± 2.7 months. A total of 52 interforaminal implants were inserted (two per patient) of the BioHorizons RMR® trademark (Biohorizons Internal Implant System) measuring 3.8 x 15 or 3.8 x 12 mm, rehabilitated with ball attachments to support the lower overdenture.
The variables were described as average, standard deviation, and range. The sagittal inclination of the implant (MI) to the mandibular plane ranged from 63.48 to 106.69°, with an average of 78.89 ± 10.9°. The results of the occlusal plane (OI) ranged from 68.41 to 100.13°, with an average of 84.75 ± 9.3°. The compensation angle (CA) was 13.94 to 82.31°, with an average of 32.21 ± 13.4°. The average value of the facial plane angle was 93.17 ± 3.4°, with a range of 86.75 - 99.19°, of which 73% corresponded to an inclination in the lingual direction (> 90°) and the remaining 27% had a vestibular direction, as shown in table 1.
Table 1 Angular variables
| N | Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|---|
| Skeletal relationship (angle of the facial plane) | 26 | 86.75 | 99.19 | 93.1719 | 3.35106 |
| Sagittal inclination of the implant (MI) (mandibular plane) | 26 | 63.48 | 106.69 | 78.8869 | 10.94114 |
| Occlusal plane (OI) | 26 | 68.41 | 100.13 | 84.7531 | 9.33855 |
| Compensation Angle (CA) | 26 | 13.94 | 82.31 | 32.2142 | 13.36408 |
Normality: angle of 90° between the occlusal (or mandibular) plane and the axis of the implant
As for the vertical variables, the anterior facial height ranged from 39.85 to 64.57 mm, with an average of 51.78 ± 5.9 mm. Symphyseal height (SH) ranged from 12.53 to 32.16 mm, with an average of 19.37 ± 4.3 mm. Initial prosthetic height (PH) ranged from 15.50 to 25.83 mm, with an average of 21.18 ± 3.0 mm, as shown in table 2.
Table 2 Vertical variables
| N | Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|---|
| Anterior facial height | 26 | 39.85 | 64.57 | 51.7815 | 5.87780 |
| Symphyseal height (SH) | 26 | 12.53 | 32.16 | 19.3746 | 4.25313 |
| Initial prosthetic height (PH) | 26 | 15.50 | 25.83 | 21.1819 | 3.01383 |
The variable of bone loss was 0.54 ± 0.4 on average, with a minimum value of 0.0 and a maximum of 1.53. The results show that denture rebasing occurred only in 15% of patients who required this procedure (Figure 2).
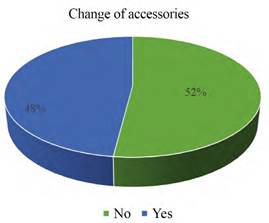
Concerning the variable of change of accessories, 52% of patients did not need any change, while the remaining 48% did need change, as shown in figure 3. Similarly, only 7.4% of patients had loosening of the prosthetic attachment (Figure 4). No significant differences could be established among variables that had few cases.
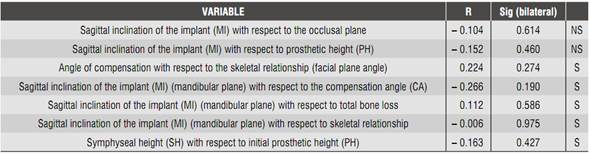
The bivariate analysis was performed between the sagittal inclination of the implant with respect to other variables, conducting the Pearson (r) correlation analysis, finding out a low but significant correlation (p < 0.05) for most variables, except for occlusal plane and prosthetic height (Table 3).
The statistical adjustment showed a moderately negative linear correlation (r = - 0.331) between the sagittal plane inclination of the implant (MI) (mandibular plane) and the occlusal plane (OI), as shown in the scatter plot (Figure 5).
Concerning the correlation between the sagittal angle of the implant and anterior facial height, there is a slightly negative relationship (r = - 0.13), as shown in figure 6.
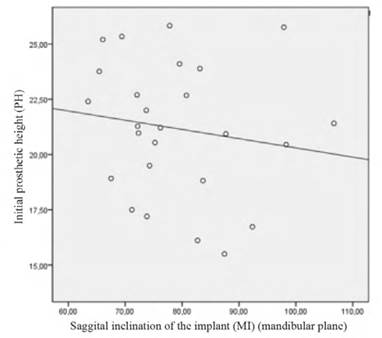
The correlation between the sagittal inclination of the implant and prosthetic height was linear and slightly negative (Figure 7).
In terms of correlation between inclination of the implant and compensation angle, a moderate negativelinear relationship was observed (r =- 0.41), as seen in figure 8.
In grouping the data by the variable of prosthesis rebasing, the average MI was higher in patients who underwent rebasing (89.70 ± 11.7°) compared to those who did not have this procedure (76.91 ± 9.8°), as shown in figure 9. Similarly, there was a strong positive correlation between MI and OI in patients who did need rebasing (r = 0.79), while those who did not have rebasing showed a low and negative correlation (r = -2.4), as shown in figure 10.
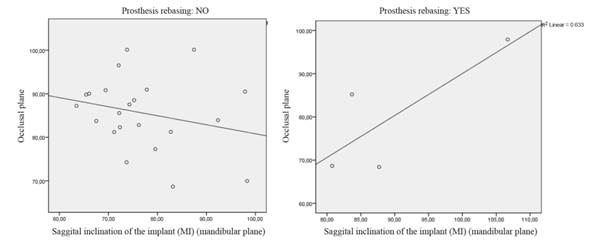
Figure 10 Correlation between inclination of the implant and occlusal plane in patients with and without prosthesis rebasing.
On the other hand, the average implant inclination in patients who didn’t undergo change of accessories was lower (77.09 ± 9.97°) compared to those who did have change of accessories (80.68 ± 9.9°), as shown in figure 10, although the differences were not significant (p = 0.73). Also, there was a high negative linear correlation (r = -0,742) between the inclination of the implant and the occlusal plane in patients who had change of accessories (p = 0.009), while those who did not have changes presented a slight negative linear relationship between the variables (r = -2.87), as shown in figure 11.

Figure 11 Correlation between inclination of the mandibular implant and the occlusal plane in patients with and without change of accessories
Student’s t test was used to determine the differences between genders, showing that the sagittal inclination of the implant was higher in males, but this difference was not significant (p = 0.337); nor was it in the occlusal plane (p = 0.731), the compensation angle (p = 0.571) or the anterior facial height (p = 0.738).
It was shown that there was a strong positive linear relationship (r = 0.74) between the inclination of the implant and bone loss, with statistical significance (p = 0.007). By grouping the results by change of accessory, the correlation was strong (r = 0.805) in those patients who did not have a change in accessory, while those who had a change in accessory showed a low correlation (r = 0.285); the first result was significant (p = 0.001) but the second was not (p = 0.457), as shown in figure 12.

Figure 12 Correlation between inclination of the implant and bone loss grouped by change of accessory.
Finally, by grouping data by skeletal classification, 48.1% of the patients were class III, 44.4% class I, and 7.4% class II. The average inclination in class I implants was 77.53 ± 9.5, in class II was 79.56 ± 2.3, and in class III was 79.19 ± 12.3; although there was variation, the differences were not statistically significant between the groups (p > 0.05). The correlations between inclination of the implant and the occlusal plane were low in the three skeletal classes.
The researchers did not conduct correlation analysis of the variable “loosening of the prosthetic attachment” because it did not have enough cases. Similarly, intragroup statistical differences were not established for the same reason.
DISCUSSION
Rehabilitation with implant-supported overdentures can be a treatment choice, although it may pose problems when the implants and the connections are not completely parallel. This leads to a decrease in retention and longevity of overdentures.(9,10,11,12,13,14,15,16,17,18,19,20) Similarly, the location and degree of the occlusal forces affect the quality and quantity of the pressures and tensions produced in all components of the bone-implant-prosthesis complex;(21) consequently, the angulation of the implant can affect the clinical outcomes. The present study aimed to evaluate the sagittal inclination of implants with respect to the occlusal plane of overdentures and its effect on the prosthetic behavior in two years of service.
In this study, lateral cephalic radiographs were used to evaluate the inclination of implants, since it is one of the most accurate ways to measuring the location of the implant in the bone structure.
Radiographs can help establish whether the implants and attachments are parallel to each other, as otherwise there would be negative consequences leading to failure of the implant, the prosthesis and the treatment in general, and thus to patient dissatisfaction.(22,23,24) In addition to the cephalometric variables associated with the location of the implant taken into account in this study, other clinical variables were analyzed, such as the need for change of accessories, the loosening of the prosthetic attachment, the need for denture rebasing, and other clinical observations that were found.
Some studies have shown that an implant inclination of up to 5° does not significantly affect the retention.(25) Hong et al(26) found that one could achieve less stress and better stability of implant-supported overdentures with two implants when these are placed parallel to the axial axis; these data were validated by Parel.(27) Schramm-Scherer et al concluded that a lingual inclination of implants to the occlusal plane is less favorable and leads to a greater loss of bone connection, primarily on the lingual site of the implant.(28) It has also been demonstrated that an inclination greater than 20° would lead to a decrease in denture retention.(29)
The results of this study demonstrate that the sagittal inclination angle may be linked to the need of rebasing and to a change of accessories, but not to the loosening of the prosthetic attachment. On the contrary, Mericske-Stern and Zarb(15) assessed the forces of implants that retain overdentures, concluding that the axis of the implant, in relation to the occlusal plane of the corresponding prosthesis, has no significant influence on the peri-implant results or on the support of the overdentures.
The results of the present study were similar to the study by Krennmair et al,(31) who proved that the sagittal inclination of the implant ranged from 53 to 96°, with an average of 74.3 ± 9.3°. In the present study, it ranged from 68.41 to 100.13°, with an average of 84.75 ± 9.3°. This difference may be explained because the individuals studied by Krennmair et al(31) were mostly skeletal class I patients (60%), contrary to the ones assessed in this study, who were mostly class III (48%); in addition, in the present study only 7% were class II, and in the study of reference this class corresponded to 18%. Both studies show that the sagittal inclination of the implant is lower in class I patients, in comparison with class III patients and much lower in class II patients. On the other hand, only one class III case was rehabilitated in this study, and all the others were rehabilitated as class I, even though skeletally they were in another classification -which can normally happen, since skeletal changes are altered by other factors, mainly age and edentulism-.
The average value of the angle of the implant to the occlusal plane was 93.17 ± 3.4°, of which 73% had an inclination towards lingual (> 90°) and the remaining 27% had a buccal orientation (< 90°), different to what was reported by another study conducted in 44 patients with implant-supported overdentures, finding out that 19% of the implants had an exact angle of 90°, 11% had a lingual inclination, and the remaining 70% had a buccal inclination.(15)
The present study showed that some clinical variables might be affected by the inclination of the implant. Notably, in patients who required prosthesis rebasing, the sagittal angle of the implant was greater (89.70 ± 11.7°) compared to those who did not have prosthesis rebasing (76.91 ± 9.8°); similarly, the ones who needed change in accessory had higher values (80.68 ± 9.9°) in comparison to those who did not require a change of accessory (77.09 ± 9.97°). This can be interpreted in the sense that an augmented sagittal inclination could produce unfavorable clinical circumstances and affect the behavior of the implant, as suggested by Atashrazm et al, who discovered that changes in angulation affect the retentive properties of overdentures.(30)
Similarly, the results showed that there was a significant correlation between the sagittal inclination of the implant and the compensation angle, which was linear, negative and moderate (r = -0.41), similar to a study in which the same variables were evaluated, finding out a significant correlation (r = -0.46); this means that the greater the sagittal inclination of the implant, the shorter the angle of compensation, which is not surprising since, as the inclination increases, there is a tendency to the verticalization of the measurements.(31)
On the other hand, diverse designs of splinted attachments for implants will differently influence the lateral retention forces and the inclination of the implant. With the different systems of fixation there was a greater lateral force, especially in cases of inclined implants. Under these circumstances, there might be an increase in mechanical risks, such as wear or fracture of fixation systems, as well as loosening or fracture of the attachments or screws.(32) Al-Ghafli et al used an experimental model to evaluate the effect of cyclic displacement in the retention of the ball attachment system for an overdenture when two implants were placed with angles of 0, 5, 10, 15, and 20 degrees, concluding that the angulation of implants affect the longevity of retention.(19)
In the present study, the accessories (either retentive plastics or rubbers) had to be changed in almost half the patients (48%); another study reported that the time needed to change retention rubbers was on average 5 to 6 months.(33) In another study on single mandibular implant-supported overdentures, in a ball attachment of larger diameter (3 mm in diameter, Nobel Biocare) there was no need to replace rubbers in 12 months,(34) suggesting that the decision to change rubbers must not be associated with time but with other factors which, with a good clinical observation, would help prevent complications.
The functional dynamics of overdentures seems to depend on the morphological characteristics of the face and mandible, the interalveolar relationship of both jaws, and the form and degree of mandibular atrophy. The functional stability of full dentures should be mainly determined by the occlusal concept; however, there are individual variations. The vertical transmission of functional forces to the implants does not seem to depend primarily on the vertical direction of the axis of implants themselves.(19)
Finally, a limitation of this study is that it analyzed a dynamic problem with a two-dimensional static method, although the method was validated by other studies that evaluated cephalometric variables, specifically the angle of inclination. A study with three-dimensional images would provide more information on other measurements that could be related to the sagittal angle of the implant. On the other hand, evaluating some clinical variables may be a complex task, since each patient has particular morphological aspects and factors associated with rehabilitation, prompting the implants to behave differently. This complexity highlights the importance of this type of studies to try to understand the treatments with implant-supported prostheses; further studies with more standardized samples are needed.
CONCLUSIONS
The average inclination of the implants of patients who did not undergo a change in retentive accessories (either plastics or rubbers) is lower (77.09 ± 9.97°) compared to those who did have a change of accessories (80.68 ± 9.9°). There was a high negative correlation between implant inclination and occlusal plane in patients who had a change of accessories, whereas those who did not have changes had a slighter correlation.
The sagittal inclination of the implant has an effect on the need for rebasing. The average MI is greater in patients who underwent rebasing (89.70 ± 11.7°) in comparison to those who did not have rebasing (76.91 ± 9.8°). Similarly, there was a strong positive correlation between the MI and the OI in those who needed rebasing (r = 0.79), while those who did not have rebasing had a low and negative correlation (r = -2.4).
The sagittal inclination of the implant has an effect on bone loss around the implants. There is a strong positive linear relationship (r = 0.74) between the inclination of the implant and bone loss, with statistical significance (p = 0.007). That is to say, the greater the sagittal inclination, the greater the bone loss, and it is also affected by any change in accessory.
The sagittal inclination of the implant influences the skeletal relationship of patients; it varies among the three classes, but the differences are not statistically significant within the groups (p > 0.05).
It could not be determined whether the sagittal inclination of implants has an effect on prosthetic fractures, or even on the loosening of the prosthetic attachment, since there were not enough cases.
RECOMMENDATIONS
The authors recommend to continue the study with the same sample and to evaluate the variables over a period of five years. They also suggest conducting additional clinical trials with a larger and more homogeneous sample in terms of age, and with a greater number of patients requiring change of rubbers, loosening of prosthetic attachment, and repair or replacement of prosthesis due to fractures.











 text in
text in