INTRODUCTION
Unilateral condylar hyperplasia (UCH) is a pathological alteration characterized by excessive and progressive growth of one of the condyles, affecting either the head, the condyle neck, the body, the mandibular ramus, or all of these, depending on its presentation.1,2,6 It appears as a self-limiting, deforming, pathological condition causing alterations in facial bone and soft tissues, as well as stomatognathic functional problems.1-5 The dentoalveolar and skeletal structures compensations happening in the presence of mandibular lateral deviation-as in the case of hemimandibular elongation UCH- include: canting of the maxillary plane and the subsequent canting of the occlusal plane by dentoalveolar supraeruption on the affected side, ipsilateral molar and canine class III dental relationships, midline deviation to the contralateral side, and cross bite or edge to edge bite on the unaffected side, with greater negative torque of the lower crowns on that side.7 According to Olate et al,8 condylar hyperplasia is the main cause of postnatal facial asymmetries. However, this condition does not have a known etiology and is influenced by genetic, traumatic, functional, hormonal, and neoplastic factors.2 Condylar hyperplasia is more common among female patients, with ratio proportions ranging from 2:1 to 7:2.9,10 Similarly, there is a higher prevalence on the right condyle in comparison to the left condyle.11,12
The proper diagnosis of UCH should be based on an accurate and thorough correlation of facial manifestations against intraoral occlusal features and radiographic or tomographic findings. Wolford et al suggested a classification system of condylar hyperplasia including several etiologic factors for hyperplasia, which help guide the treatment plan.13 The classification has 4 types, with type 1 being the most common: Type 1: hemimandibular elongation caused by increased growth of the condyle during puberty-subdivided into bilateral and unilateral, with horizontal growth predominance-; Type 2: elongation caused by pathologies such as osteochondroma-subdivided into horizontal and vertical growth vector-; Type 3: elongation associated with benign tumor processes causing condylar hyperplasia; Type 4: elongation associated with malignant tumor processes.13 Once the diagnostic impression has been established, and with suspected active hyperplasia, SPECT (single photon emission computed tomography) bone scintigraphy is ordered to determine the active or passive stage of the hyperplasia.2,12,14-16
The treatment indicated in the presence of active condylar hyperplasia is high condylectomy of the affected condyle, sectioning about 6 mm of condyle height from medial pole to lateral pole by a preauricular approach,17 although larger condylectomies proportional to the asymmetry have been reported.18 Even if the active stage of the pathology has stopped, morphological changes remain in the three planes of space according to the severity of the hyperplasia, the age in which it was detected, and the time it was in active stage. The treatment of these morphological alterations becomes an orthodontic challenge when one chooses to compensate this dentoskeletal alteration orthodontically, instead of subjecting the patient to a second surgical procedure to correct the secondary asymmetry through orthognathic surgery.
The Multiloop Edgewise Arch Wire (MEAW) technique, developed by Sato et al7 and used by Kim and Han among others,19 helps make individual vertical movements in the posterior area, and collective movements in the anterior area. This technique provides the biomechanical possibility of performing posterior extrusion on the displaced side, which is the one with the smallest vertical dimension, and performing class III mechanics on the affected side with molars verticalization to achieve dentoalveolar compensation (Figure 1). Extracting the third molars eliminates posterior discrepancy and allows molar verticalization and intrusion. This last step is intended to improve the remnant mandibular lateral deviation following condylectomy, correct the occlusal canting, and provide adequate occlusion.19-21

Figure 1 Multiloop archwires for occlusal plane control and use of class III elastics on the affected side and class I elastics on the displaced side. Note individual bends for vertical movement in the posterior area, allowing dentoalveolar compensation such as extrusion of posterior teeth on the displaced side, which is the one with the lowest vertical dimension
The purpose of this series of cases is to present our diagnostic and treatment protocol for UCH, where postsurgical dentoalveolar correction was performed with the MEAW technique aimed at extruding the deviated side and uprighting and intruding the molars on the affected side.
DESCRIPTION OF CASES
A series of three patients (one woman and two men) presenting active UCH -two cases of left lateral deviation due to right condylar hyperplasia and one case of right lateral deviation due to left condylar hyperplasia- corroborated with SPECT (radiopharmaceutical hypercaptation in the affected condyle above 55% with respect to the contralateral condyle) were subjected to high condylectomies to stop the active state of the disease. Subsequently, they were treated with the following post-surgical orthodontic protocol: prior to surgery, the brackets were adhered, placing the first alignment and leveling arch and extracting the third molars.19 One week after surgery, the MEAW arches were placed. In subsequent visits, the arches were activated with extrusion folds on the displaced side and the use of class I (vertical) or class II elastics of 3/16 and 6.5 ounces, as needed. A tip-back for posterior teeth and intrusion folds for first and second molars with class III elastics were performed on the operated side, in order to compensate for facial asymmetry and occlusal canting. Patients were treated for 17.8 months on average. All patients provided an informed consent to carry out the procedures.
Case 1
15-year-old male patient with dental malocclusion Class III, right subdivision, and Class II, left subdivision, with Class III skeletal relationships due to left mandibular displacement associated with a right condylar hyperplasia. Dentally, he showed maxillary alveolar protrusion and slight upper and lower crowding. Facially, he had a dolichofacial biotype, a concave profile with the lower third severely increased and mandibular prognathism (Figure 2).

Figure 2: Patient #1 initial records of. Profile photograph (A), frontal photograph (B), smile photograph (C), frontal intraoral photograph (D), right side photograph (E), left side photograph (F), upper occlusal photograph (G), lower occlusal photograph (H). lateral X-ray of the skull (I), postero-anterior radiograph (J), panoramic X-ray (K)
The MEAW technique was performed after the surgical procedure, with vector Class III elastics on the right side and class I (vertical) on the left side (Figure 3). The case was completed with bilateral Class I molar and canine relationships, suitable static and dynamic occlusal relationships, 2 mm overjet and 30% overbite in 16 months (Figure 4).
Case 2
13-year-old female patient with Class III dental malocclusion and Class III skeletal relationships due to severe mandibular right displacement associated with left condylar hyperplasia. Dentally, she had moderate proclination of upper incisors, mild proclination of lower incisors, and slight upper and lower crowding. Articularly, the patient had bilateral painful symptoms at maximum opening in both TMJ’s. Facially, she a had a mesofacial biotype, straight profile, biprochelia and mandibular macrognathism (Figure 5).

Figure 5: Patient #2 initial records. Profile photograph (A), frontal photograph (B), smile photograph (C), frontal intraoral photograph (D), right side photograph (E), left side photograph (F), upper occlusal photograph (G), lower occlusal photograph (H). lateral X-ray of the skull (I), postero-anterior radiograph (J), panoramic X-ray (K)
The MEAW technique was performed (with brackets Synthesis®, Ormco Corp., Orange, CA) with vector Class I (vertical) elastics on the right side and Class III elastics on the left side (Figure 6). The case was completed with an adequate transverse occlusal relationship, Class I molar and canine bilateral relationships, and adequate overjet and overbite in 22 months (Figure 7).

Figure 6: Patient #2 intermediate records. Intraoral frontal photograph with MEAW arches (A), right side photograph with Class I elastic (B), left side photograph with class III elastic (C). Panoramic X-ray (D), TMJ X-ray with open mouth and closed mouth (E), posterior-anterior radiograph (F)
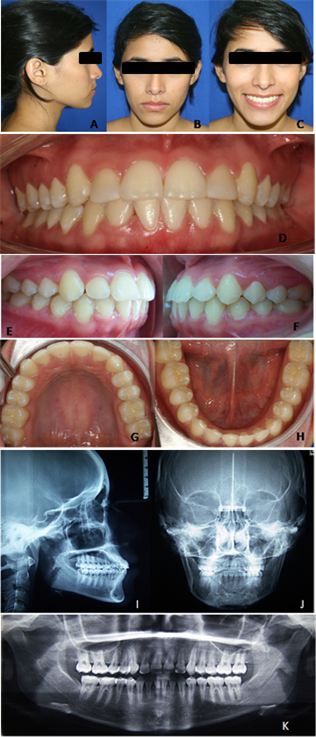
Figure 7: Patient #2 final records. Profile photograph (A), frontal photograph (B), smile photograph (C), frontal intraoral photograph (D), right side photograph (E), left side photograph (F), upper occlusal photograph (G), lower occlusal photograph (H). lateral X-ray of the skull (I), posterior-anterior radiograph (J), panoramic X-ray (K)
Case 3
20-year-old male patient with dental malocclusion Class III, right subdivision and mild Class III skeletal relationships associated with a mild maxillary retrognathism and left lateral mandibular displacement due to right condylar hyperplasia. Dentally, he had upper wide spacing and slight proclination of upper incisors. Facially, the patient had a straight profile with a mesofacial biotype (Figure 8).

Figure 8: Patient # 3 initial records. Profile photograph (A), frontal photograph (B), smile photograph (C), frontal intraoral photograph (D), vertical overbite photograph (E), horizontal overbite photograph (F) right side photograph (G), left side photograph (H), upper occlusal photograph (I), lower occlusal photograph (J). Posterior-anterior radiograph (K), lateral X-ray of the skull (L), panoramic X-ray (M).
The treatment protocol with the modified MEAW technique was conducted using Class III elastics on the right side and Class II elastics on the left side (Figure 9). The case was completed in 18 months with bilateral molar and canine Class I dental relationships, adequate static and occlusal dynamics relationships, and correct overjet and overbite (Figure 10).

Figure 9: Patient #3 intermediate records. Profile photograph (A), frontal photograph (B), smile photograph (C), frontal intraoral photograph with MEAW arches (D), right side photograph with class III elastic (E), left side photograph with class II elastic (F)
DISCUSSION
In our therapeutic approach, all UCH cases were previously documented thorough a clinical analysis, along with diagnostic aids such as panoramic radiograph, posterior-anterior radiograph, lateral X-ray of the skull, SPECT bone scan, and follow-up photographs. As stated in previous studies,1,9,13,22-24 appropriate diagnosis is necessary to start correcting the pathology and its anatomical alterations in an ideal and effective way. Diagnostic aids are key to achieve this goal, and all of them are required in the diagnosis of mandibular dismorphogenesis. However, the correlations with clinical variables is what provides the greatest amount of information in the diagnostic of unilateral condylar hyperplasia.18 In our case, the average age for starting treatment was 15.3 years. According to the literature, condylar hyperplasia diagnosis is most commonly established in the ages of 12 to 30 years, with an average of 25.8 years.10-12,16 Nitzan et al claim that a third of all patients are diagnosed before the age of 20.10
Hodder et al (2001)16 suggest a therapeutic algorithm based on the results of the SPECT bone scintigraphy and the severity of the patient’s aesthetic compromise. In their study, a condyle radiopharmaceutical captation score of ≥ 55% in relation to the contralateral condyle was indicative of active hyperplasia and therefore of high condylectomy, but only in the presence of severe facial compromise. Otherwise, waiting for a new control scan is recommended to allow the asymmetry to progress towards a true skeletal discrepancy.16 Elbaz et al (2014)9 propose to differentiate functional-driven mandibular lateral deviation from condylar hyperplasia. Although hemimandibular elongation-the most common form of condylar hyperplasia-is very similar to the functional-driven mandibular lateral left deviation, its etiology is totally different. The former shows remnant activity of precartilaginous cell growth of the condylar growth zone, causing imbalance between cell growth, extracellular matrix production, and endochondral ossification.9,25 The latter shows mandibular lateral displacement from premature contact or due to interference. The authors also suggest performing the correction of asymmetry at the expense of the condylectomy and orthognathic surgery, placing little importance on the orthodontic treatment.9 Wolford et al (2014)13 propose a treatment protocol based on the classification of the asymmetry. This protocol requires surgical intervention of the condylectomy, disc replacement, condylar neck re-contouring in cases of active hyperplasia, and orthognathic surgery once condylar growth has stopped or is in an inactive phase. In types 3 and 4-in which asymmetry is caused by tumor processes-the bone mass is removed, reconstructing the structure with personalized implants, depending on the size and type of pathology.
While taking into account the three-dimensional alterations of the UCH, these approaches are of a surgical nature only. It is necessary to determine the orthodontist’s intervention times, according to the active or passive state of the hyperplasia, in order to achieve an adequate facial and occlusal balance, in these cases: if the diagnosis of active hyperplasia was made in early stages when no alterations had yet been produced; if it was done at an intermediate stage with alterations in the three planes of space, but with the possibility of orthodontic dentoalveolar compensation, or if it was a late diagnosis with no possibility of dentoalveolar compensation, and therefore orthognathic surgery is the most appropriate treatment to correct the asymmetry, all under a multidisciplinary scheme.
In the active UCH process, high condylectomy is the indicated and immediate treatment once diagnosis has been made. But post-surgical orthodontic intervention should be quick and effective, aimed at either correcting malocclusion in early diagnostic cases, making dentoalveolar compensation with vertical management in cases of intermediate diagnosis, or performing orthodontic decompensation in order to prepare for orthognathic surgery in cases of late diagnosis.
The MEAW therapeutic approach helps treat non-severe asymmetries-either functional asymmetries or secondary UCH alterations-as it enables individual movements in customized wires and the use of elastics that help guide mandibular positioning. However, some reports suggest that the straight archwire technique and the use of temporary anchorage devices (TAD’s) can be used to perform differential intrusion and extrusion procedures, achieving good results in the correction of canting and asymmetry secondary to surgery.26,27 This alternative treatment has the same approach as the MEAW technique but requires bone-supported devices on the affected side to achieve intrusion of the maxillary posterior sector without producing this effect on the mandible.
Comparing both orthodontic treatment schemes, our proposal was able to produce dentoalveolar changes in the four quadrants, with excellent patient cooperation in the use of intermaxillary elastics. It was imperative to start the active phase of the orthodontic correction as soon as possible, aided with elastics to achieve adequate occlusal stability and guide the condyle healing in a posterosuperior position and in a correct relationship with the articular tissues. This procedure was carried out because, after the condylectomy, patients usually have an open bite more pronounced on the displaced side, due to the decrease in the vertical dimension of that side, coupled with the hemarthrosis of the surgery and the action of the upper beam of the external pterygoid, which displaces the condyle downwards and forwards. Techniques using temporary anchorage devices substantially reduce the need for patient cooperation, which is an advantage in the development of treatment. However, the authors report that during the retention phase, 3/16 elastics should be used between the temporary anchorage devices of the treated sector for 1 year to ensure stability.28
The traditional form of the MEAW technique proposes to use standard brackets without prescription, with 0.018" x 0.025" slots and blue Elgiloy arches 0.016" x 0.022" (Rocky Mountain Orthodontics, Denver, CO). However, in this proposal the three patients were treated with preadjusted brackets with 0.022" x 0.028" slots, one of them with active self-ligation. All the patients were treated with MEAW arches built in blue Elgiloy 0.019" x 0.025".27,28 The fact that the use of different brackets yielded the expected results suggests that the mechanical element that stimulates dental movement is the activation of the multi-loop arch to manage the vertical dimension and to control the occlusal plane, while the brackets act as the receiving element of such activation and as vehicle of expression towards the periodontium. It is very important for clinicians to know the structural and design characteristics of the brackets they use to obtain the desired movement.
CONCLUSIONS
The proper diagnosis of UCH should be made from a thorough correlation between extraoral and intraoral clinical findings and radiographic or tomographic findings, to later define the active or passive stage of the pathology by SPECT.
Proper diagnosis allows a timely treatment plan in which orthodontic management prevents the progression of deformities associated with UCH.
The dentoalveolar compensation with vertical management achieved with the MEAW technique for non-severe cases of asymmetries is an effective therapeutic approach in the correction of occlusal canting and left mandibular displacement.
It is important to carry out prospective studies of cases with facial asymmetries to assess the level of stability of this therapeutic proposal.











 text in
text in 





