INTRODUCTION
Pythiosis or oomycosis is known in Colombia as “spurious or ficomycosis” 1; In Brazil, as “ferida brava, mal dos pântanos y ferida de moda” 2; In other parts of the world, such as “granular dermatitis, Florida leeches, Gulf Coast fungus, bursatee and hyphomycosis” 3. It is a granulomatous disease of the cutaneous and subcutaneous tissue caused by Pythium insidiosum4.
Cardona et al 5 affirm that Pythiosis particularly affects wounds in the limbs, mouth and chest; Being attributed to the fact that these areas are more exposed to the oomycete, causing a marked and rapid inflammatory response in the skin of the region of the limbs. The lesion is characterized by the formation of severe granulomatous and granulocytic ulcerations and elevations with irregular crater-like borders. The size of the lesions depends on the location and the time of evolution of the infection and can be measured between 12 and 50 cm in diameter, with the presence of the fistulous plugs or cavities formed by the oomycete in its invasive process in the granular tissue. After injury, the dead cells behave like a foreign body, triggering the inflammatory response of the body in order to promote its phagocytosis and to allow the subsequent repair of the affected tissue.
The presence of necrotic masses and calcifications that easily detach, with white-yellowish coloration, whose dimensions vary from 2 to 10 millimeters in diameter, containing hyphae and the infiltrate of eosinophils called “kunkers”, with plates and fistules and fibrinous-bloody Discharge, are unmistakable signs of Pythiosis 6.
Histopathologically, there is an intense proliferation of irregularly arranged connective tissue, many fibroblasts and a marked piogranulomatous inflammation, with intense infiltration of eosinophils, followed by neutrophils, the presence of a multifocal mass and the Splendore Hoeppli phenomenon. Hyphae are visible in silver staining of Grocott’s methanamine, where branched, occasionally septate, dark brown, smooth and parallel walls with a size of 2.6 - 6.4 μm are observed, sometimes forming 90 ° angles 7.
There are reports in the literature of various therapies aimed at eliminating the etiological agent of the disease (P. insidiosum), to improve tissue quality and promote tissue repair. Despite the use of antimycotics as a treatment option, there are few studies with favorable results, with unconvincing evidence of treatment efficacy in cutaneous granuloma due to pythiosis 8.
Triamcinolone acetonide has not been used in skin disease therapy and even less in equine cutaneous pythiosis cases, this is why this study aimed to evaluate the therapeutic therapy of this drug by means of studies Histological and histochemical.
MATERIALS AND METHODS
Ethical aspects. For this study naturally infected horses clinically and histopathologically diagnosed with cutaneous pythiosis were used. The study was approved by the Ethics Commission on Animal Use (CEUA) of the Federal University of Viçosa (UFV), process N ° 74/2012. Animals have not been subjected to processes that develop unnecessary pain andor stress. The animals were immobilized considering the technical handling and animal subjection regulations, framed under the fulfillment of the Universal Declaration of Animal Rights, referring to the international ethical principles for biomedical investigation with animals of CIOMS International Organizations of Medical Sciences) established by UNESCO (United Nations Educational, Scientific and Cultural Organization) and WHO (World Health Organization) of 1949 and Law 84 of October 27 of 1989 (Colombian Animal Protection Statute) 9.
Location. The experiment was carried out on the Caribbean coast of Colombia, in the department of Córdoba, located between coordinates 7° 23‘and 9° 26’ latitude north and 74° 52‘and 76° 32’ longitude west of the Greenwich meridian, At a height of 30 meters above sea level, average annual temperature of 28°C, relative humidity of 82%, average annual rainfall of 1,400 mm and tropical forest climate, with two well-defined seasons 10.
Animals. 24 horses were used, of both sexes, different ages and average weight of 380 kg. Inclusion criteria based on the presence of clinical cutaneous pythiosis, diagnosed by general physical examination and confirmed by histopathology. During the study of the animals were kept in pasture, with grass and water ad libitum.
Two research groups of 12 animals each were used. A group of animals with Pythiosis received intramuscular treatment with 50 mg of triamcinolone acetonide for 3 applications every 15 days (treated group - GT). In the other group of animals with pythiosis no treatment (control group - GC) was applied. Tissue biopsies were collected from the periphery of the granuloma in all animals of the study every four days until the total cure of the granuloma in the GT was achieved.
Methodology. The animals were divided into two groups of 12. The first group (treated group - GT) received intramuscular treatment with 50 mg of triamcinolone acetonide every 15 days to complete three applications. No treatment was applied to the second group (control group - GC).
Tissue biopsies from the periphery of the lesion with 6-mm punch were collected in all animals of the study, with sedation (Acepromazine 1%, Zoo®, Colombia) and local anesthesia (Lidocaine 2%, Synthesis®, Colombia) ; The samples were taken every four days until the total cure of the granuloma in the GT was achieved.
The samples were placed in 10% formalin for 24 hours and processed until their inclusion in paraffin according to the routine protocols of the histopathology laboratory of the University of Córdoba. Subsequently, they were transferred to the Laboratory of Structural Biology of the Department of General Biology of the Federal University of Viçosa, Brazil, where they were processed for histopathological and histochemical evaluation. Cut to 5μm thickness in a microtome (Leica RM2125 RTS ®, Japan) and stained with Hematoxylin - Eosin (H & E), Gomori Trichrome (TG), Picrosirius Red / Polarization (PR / P), Silver Grocott Methanamine Grocott’s Methenamine Silver) and Schiff Periodic Acid Schiff (PAS). A polarized light microscope (Olympus BX-53®, Japan) from the Laboratory of Molecular Systematics / BEAGLE of the Department of Animal Biology of the Federal University of Viçosa, Brazil was used for the sample analysis.
RESULTS
Histopathological and histochemical analyzes confirmed the diagnosis of cutaneous Pythiosis in the 24 horses of the study, according to what was reported as a diagnostic method 2,5,6,7,11,12.
In the H & E staining, intense proliferation of irregularly arranged connective tissue, numerous fibroblasts and collagen fibers, and marked piogranulomatous inflammatory infiltration were observed, with intense infiltration of polymorphonuclear cells (PMN), mainly eosinophils and neutrophils followed by macrophages in Lower proportion and with diffuse distribution, presence of multifocal necrotic masses and Splendore Hoeppli (SH) phenomenon, which corresponds to a multifocal diffuse eosinophilic piogranulomatous dermatitis (Figure 1). Similarly, in the GMS staining, branched, occult septate, dark brown structures with smooth and parallel walls of 2.6 - 6.4 μm, sometimes forming 90 ° angles, were observed. These correspond to intralesional pseudohifas characteristic of oomycete P. insidiosum (Figure 2). PAS staining was negative for oomycetes and fungi.

Figure 1 H & E staining. Diffuse granulomatous multifocal dermatitis with marked piogranulomatous inflammatory infiltration, intense PMN infiltration, presence of multifocal necrotic mass or Splendore Hoeppli phenomenon (arrows), and absence of granuloma-side epithelium (AEP). 10X.

Figure 2 GMS coloration. See the occipital, right-angled, branched, dark brown structures with smooth, parallel walls corresponding to hyphae of Pythium insidiosum. A.) 20x. B.) 40x.
Regarding wound recovery, all GT granulomas treated with triamcinolone acetonide were found to be 100% recovered, however, all wounds from CG animals remained the same or increased throughout the study.
In HE staining in all tissue biopsies of the 24 equines of the study, similar histopathological features were initially observed. However, when comparing the tissue samples from the two groups (GT and GC), it was observed that in GT as the granuloma recovery progresses, the inflammatory process from an intense (III) to moderate degree (IIM) ) And mild (IIL), evidenced by the progressive decrease of PMN, fibrin and SH phenomena, as well as the increase of newformed blood vessels (VS), connective tissue (TC), hair follicles (PF), sebaceous glands And in partial progressive re-epithelialization (REpP) with formation of epithelial crypts (EC) until complete re-epithelialization (REpC) of the granuloma area was achieved (Figure 3), whereas the CG presented diffuse granulomatous dermatitis Multifocal with intense inflammatory infiltrate, focal edema and congestion, as well as absence of epithelium and formation of a leukocyte fibrinotic layer throughout the study.

Figure 3 Coloration of H & E in GT. A.) Periphery of the granuloma on day 0 of the study, where the healthy side (LS) is differentiated from the diseased side (LD). The presence of the epithelium, sebaceous glands and follicles may be observed in the LS, whereas in the LS there is evidence of PLE with formation of CFL, III (arrows) and presence of loose and unorganized collagen fibers. 4x. B) Granuloma periphery at 16 days, note the process of REpP with EC formation, as well as presence of IIM, discrete focalized congestion, neoformation of some VS and increase of CT showing the transition between granulation and tissue remodeling (arrow) . 10x. C.) At 32 days. Note the higher CT formation with more organized collagen and a great number of fibroblasts and a greater neoformation of VS and IIL, indicating an adequate remodeling process. 10x. D.) At 64 days, observe the presence of REpC and adequate amount of FP, GS, VS, TC and organized and dense collagen fibers indicating repaired skin. 10x.
In PR/P staining, a homogeneous mixture of colors characterized by areas of reddish and green-yellow birefringence was initially observed in the polarization of all 24 equine biopsies with Pythiosis, indicating the presence of mature type I collagen (Bright red in polarization) and type III (bright green-yellow in polarization) in equal proportions, with the thinner and less organized type III collagen fibers. When comparing the two groups, it can be observed that in GT, as the healing process progresses, there was an increase in type III collagen, this effect being evidenced by the change in coloration of the collagen towards green-yellow at approximately 15 days. Subsequently, at 30 days after treatment, the areas of birefringence of type III collagen were gradually replaced by type I collagen, evidenced by the change of coloration towards reddish yellow (Figure 4).
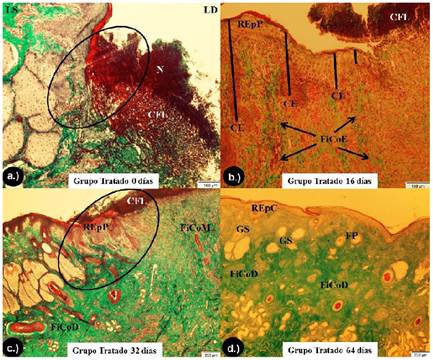
Figure 4 GT coloration in GT. A.) Periphery of the granuloma at 0 days from the beginning of the study, where the healthy side (LS) is differentiated from the diseased side (LD). In the LS, the marked formation of organized and dense collagen fibers can be observed, whereas in the LD, the absence of epithelium with formation of CFL without re-epithelialization process (circle), as well as areas of necrosis ( N) and areas without presence of collagen fibers and other areas with loose and unorganized collagen. 10X. B.) Periphery of the granuloma at 16 days. Notice the process of REpP with formation of CE (bars), as well as formation of loose and disorganized FiCoE (arrows). 10X. C.) Periphery of the granuloma at 32 days. Observe the process of re-epithelialization developing and invading the CFL (circle), and the formation and organization of FiCoM 4X. D.) At 64 days, observe the presence of REpC and adequate amount of FP, GS and FiCoD indicating a repaired skin. 4X.
At the end of the healing process, which occurred completely at 60±3.4 days, type I collagen was observed, evidenced by the predominance of bright red birefringence, which characterizes a healing process as a whole. In the same way, the type I collagen fibers become thicker, more organized and with greater birefringence, whereas in the GC the process initially observed, it was maintained throughout the study, without showing alterations in the healing process (Figure 5).

Figure 5 PR/P coloration. Photomicrographs obtained on polarization microscopy showing the distribution of collagen fibers in the scar tissue at days 0, 16, 32 and 64. A.) GC. Note the areas of reddish and green-yellow birefringence in similar proportions throughout the study. 20X. B.), C.) E d.) Group treated with triamcinolone acetonide. Note the distribution of collagen fibers in the scar tissue, indicating a change of birefringence areas predominantly green-yellow at 16 days, red-yellow at 32 days and red at 64 days. 20X.
In the GMS staining, the presence of oymytum P. insidiosum hyphae was evidenced in large quantities in all tissue samples of the 24 equines of the study. Therefore, when comparing the tissue samples of the two groups (GT and GC), no GT was observed, as the granuloma recovery progresses up to the second week, the presence of intra-lesional hyphae (16 days) progressively decreases (Figure 6), whereas in the CG the evident presence of intra-lesional hyphae was observed throughout the study.

Figure 6 Coloring of GMS in GT. A.) 4 days after the beginning of the study. It is possible to observe the presence of dark brown, occasionally septate, branched structures, with smooth and parallel walls and sometimes forming right angles, corresponding to hyphae of P. insidiosum (arrows). 20x. B.) 8 days after the beginning of the study. Note the moderate decrease in the number and size of hyphae (arrows). 20x. C.) 12 days after the initiation of the study. Observe the scarce and localized presence of hyphae, being much more difficult to find them in the tissue (arrows). 20x. D.) 16 days after the beginning of the study. Observe the small amount of hyphae in the tissue, short and more difficult to visualize in the histological evaluation (arrows). 20x.
DISCUSSION
There are no reports in literature consulted on the use of triamcinolone acetonide in investigations FOR the treatment of skin diseases, and none in the specific case of equine cutaneous pythiosis, thus, this study becomes the first work evaluating the Therapeutic response of triamcinolone acetonide using techniques with high specificity and sensitivity such as histopathology and histochemistry that will provide important information on the healing process in equine cutaneous pythiosis.
The results obtained in this study were satisfactory with 100% recovery at 60 ± 3.4 days after treatment in all WG animals, while Frey et al 13 reported a 50% recovery using the Pitium- Vac associated with curettage of necrotic material from lesions or surgery. Likewise, Pereira et al. 14 tested in vitro carposfungin (a β-glucan synthesis inhibitor) with a 63% action, while during the in vivo testing in an experimental model in rabbits, showed reduction of lesions, but when the treatment was suspended, Lesion growth restarted.
On the other hand, Argenta 15 and Cavalheiro et al 16 demonstrated in vitro studies where terbinafine was active when tested alone, showing a minimum inhibitory concentration (MIC) and minimal fungicidal concentration, since voriconazole and itraconazole were Inactive against the tested isolates. When testing the combination of voriconazole with terbinafine and itraconazole with terbinafine, they were synergistic on 17% of the samples. Similarly, Biava et al. 17 reported unsatisfactory results and less than 25% of recovery in studies where amphotericin B, 10% sodium and potassium iodide, flurocytosine, ketoconazole were evaluated, in association or not with surgery, as well as systemic amphotericin B combined with gauze pads embedded in amphotericin B and dimethylsulfoxide (DMSO) solutions.
The unsatisfactory results of traditional antifungal drugs can be explained by the inability of P. insidiosum to produce steroids in the plasma membrane, such as ergosterol, which is the albo-action component of most antifungal drugs, which in fungi, alter the permeability of the cell membrane causing cell lysis of the fungus 8,18.
Loreto et al 19 evaluated the in vitro susceptibility of P. insidiosum to Macrolide and Tetracycline antibiotics reporting some degree of inhibitory action, reducing the incorporation of amino acids into proteins, inhibiting protein synthesis and amino acid transport. There is a lack of research in sick animals naturally infected with pythiosis.
On the other hand, surgical intervention as part of the treatment for pythiosis, requires removal of the entire affected area, with a safety margin to avoid relapses, however, this is hampered by compromised anatomical structures, mainly in the limbs 20.
After contact of P. insidiosum with the host, a germ tube is formed which mechanically penetrates the tissues where the hyphae of the agent produce exo-antigens that are presented to the antigen-presenting cells (APCs). APCs secrete interleukin 4 (IL-4) which directs T helper naïve (Th0) lymphocytes into T helper 2 (Th2). The high number of eosinophils de-granulates around the hyphae of P. insidiosum are mainly responsible for the extensive and rapid tissue damage found in pythiosis and induce the development of the Splendore-Hoeppli (SH) reaction. It is suggested that the SH phenomenon and the exo-Ags secretion are evolutionary strategies developed by P. insidiosum to assure its proliferation in a host tissue 21,22.
A possible pharmacological explanation for the recovery of horses with pythiosis treated with triamcinolone acetonide is found in the immuno-modulating activity of glucocorticoids, since it inhibits the synthesis, release and / or action of cytokines and other mediators that promote the inflammatory or immune response. These molecules include pro-inflammatory cytokines, such as IL-1, IL-6 and tumor necrosis factor alpha (TNF-α), clonal expansion and IL-2, subset of helper T lymphocytes (Th1), IL-12 and gamma Interferon (IFN-γ) and, to a lesser extent, or subset Th2, IL-4 and IL-5, colony-stimulating factors such as granulocyte-macrophage colony-stimulating factors (GM-CSF), chemokines as RANTES and MIP-1α, adhesion molecules such as ICAM1, ELAM-1 and E-selectin, inflammatory mediators such as bradykinin, histamine, eicosanoids and nitric oxide, as well as molecules involved in the presentation of antigen and major histocompatibility complex (MHC) class II.
The entire spectrum of molecular albs explains both pleiotropy and anti-inflammatory and immuno-modulatory force. That is why, by blocking the synthesis of the cytokine IL-5 and granulocyte-macrophage colony-stimulating factor (GM-CSF), the programmed death of these cells (apoptosis) is triggered, which decreases the half-life of Eosinophils. Once this cytokine is responsible for eosinophilopoiesis, the function of mature eosinophils increases, as well as de-granulation, adhesion and cytotoxicity, thus prolonging the survival of that cell 23,24.
AT decreases the half-life of the eosinophil by blocking the synthesis of IL-5 and granulocyte-macrophage colony stimulating factor (GM-CSF), triggering the apoptosis of these cells, and thus Pythium is exposed to neutrophils And macrophages, which completely eliminate the hyphae in the tissue, stimulating the physiological repair of the wound. Additionally glucocorticoids prolong the survival of the neutrophils and decrease the apoptosis of these cells 25.
In the healing process, many cell types are involved whose interrelationships are regulated by the cytokines, the extracellular matrix (ECM) and the metalloproteinases (MMPs) of the extracellular matrix. In a chronic wound as the antigenic stimulus disappears, skin healing is activated allowing the reconstruction of the stratified epithelium (the epidermis), the epidermal dermal junction and the dermis, as well as its vascularization 26. After treatment with AT in the GT, the reconstitution of the tissue begins, with the accumulation of fibroblasts in the center of the wound, and initiates the synthesis of collagen and a provisional extracellular matrix.
Fibroblasts undergo a series of phenotypic changes, initially adopting a migratory phenotype, then a pro-fibrotic phenotype (as they produce collagen I, III and VI) and subsequently, adopting the myo-fibroblast phenotype, rich in actin microfilaments in the cytoplasmic side of the membrane to establish cell-cell (adherent) junctions. These cells produce the necessary new MEC for the supporting cells and blood vessels, provide nutrients and oxygen necessary for cell growth and proliferation 27. The cytokines TGF-β (transforming growth factor beta) and PDGF (platelet-derived growth factor) stimulate fibroblasts to produce collagen and other ECM components. Simultaneously, fibroblasts and endothelial cells begin to migrate on the provisional matrix in the wound space with the help of MMPs (extracellular matrix metalloproteinases), which are regulated by keratinocytes and macrophages at the wound border. The degradation of the ECM components by MMP is necessary to remove and rearrange provisional matrices and allow migration, providing formation of new blood vessels in the wound bed. An important cytokine that promotes this migration is IL-1, which stimulates the release of MMPs and synergistically induces collagenase activity in relation to IFN-γ and TNF-α. Increased levels of IL-1, therefore, may result in ECM degradation and delaying wound repair 28.
Collagen is a fundamental component in the tissue repair process, and it is synthesized from fibroblasts and present in abundance in the proliferative phase and remodeling of the wound. The most expressive types of collagen in the healing process are types I and III. Collagen III appears primarily in the wound. It is characterized as young or immature collagen and confers a disorganized appearance to the fibers. Already type I or mature collagen, replaces type III in old scars and is characterized by a greater organization of fibers 29.
Because there are many factors that affect the action of drugs in the diseased animal, such as pH, vascularization, fibrosis, idiosyncrasy, variations in the species, tolerance, sensitivity, nutritional status and body condition of the animal 30, It is necessary to carry out further studies in naturally infected animals considering AT in isolation or in combination with other therapeutic options, such as antiglycans of the latest generation inhibitors of β-glucan synthesis or antibiotics inhibitors of P. insidiosum protein synthesis.
In conclusion, the results obtained in this study showed that triamcinolone acetonide was effective in the repair of wounds of granuloma by pythiosis, showing up in the histopathological evaluation a tissue repair, and absence of the oomycete P. insidiosum in the tissue. The use of triamcinolone acetonide as a good therapeutic alternative in the treatment of equine cutaneous pythiosis may be recommended.














