Introduction
In general terms, the maintenance of industrial facilities has been considered a burden on the organization’s main activity, identified, and considered by top executives as general costs in financial balance sheets. This circumstance changed from the Second World War onwards with the automation and growth of fixed costs; with the adequate, efficient, daily use of productive resources acquiring great importance. Given this new scenario, the term maintenance came into vogue with the OECD International Congress of 1963, with the definition as “the business function that is responsible for the constant control of facilities and equipment, in addition to all the repair and revision work necessary to ensure the regular operation and good state of conservation of the productive facilities within the organization” 1.
According to the above definition, good management of maintenance leads to efficiency in organization production, making it a positive service in healthcare infrastructure. Healthcare engineering professionals, who are also responsible for the training of medical personnel, must apply these conservation and maintenance techniques. Therefore, it becomes necessary to systematize maintenance in healthcare centers by examining the current systems and incorporating those that lead to the achievement of objectives in a more effective way 2. At this point, adequate maintenance turns out to be a significant cornerstone within the organization’s infrastructure, being the Health Institutions (HI) under study in the present work. Some decades ago, when hospitals operated exclusively based on doctors’ knowledge and skills, at that time their installation and equipment systems were reduced to what was necessary for minimal activities, maintenance represented merely the process of cleaning and replacing damaged equipment, responsibilities taken on by the organization’s jack-of-all-trades 1. However, the evolution of electrical services, electronic services, biomedical equipment, infrastructure, and others, as well as the value of these in the treatment of the patient and in the operational economy justify the relevance now ascribed to maintenance problems and hospital facilities management.
This new perspective has led to the development of different methodologies and disciplines in different industrial sectors, mainly those coming from the production and reliability of energy and oil setting. There are disciplines that demonstrate reliability, availability, and organizational efficiency with a holistic view of the institutions, and that satisfactorily fulfill the objectives, strategies and policies of the organization, especially in the case of health institutions. One of the newly emerging disciplines is Asset Management (AM), originating from the United States of America, and defined as: "the coordinated activity of an organization to generate value of the asset”, with the definition of an asset being “an item, thing, or entity that has a potential or actual value in an organization.” Physical assets assume an important role in organizations, within the five types of assets: financial, human, intangible, information, and physical 3.
In this study, the authors focus exclusively on physical assets (infrastructure), considering the other categories when they have a direct impact on the physical asset management. Similarly, human factors, such as motivation and culture will be considered, which are not directly related to physical assets, but are fundamental for the satisfactory management of the whole organization 4. Also, AM has a systemic approach 5, that covers all areas of the organization to bring an effective solution to the management of industrial assets (such as improving the equipment and personnel’s productivity; optimizing maintenance resources; increasing inventory efficiency and focusing on management as a system to avoid operational stops). This operational approach leads to the discovery of unknown profits and enables better future decisions that enhance profitability and asset performance management.
Healthcare physical assets (in this case the infrastructure) may represent the most important investment for HI, given that engineering and architectural disciplines are fundamental to reform and transform the organizational structure. The adequate use of these disciplines can pave the way for patients’ recovery in the organizational climate and the community in general 6. In any case, the hospital infrastructure represents the mission, values, and principles of the organization. For this, it must be intentionally built, maintained, and operated to achieve its specific objectives, working on maintenance, investments and internal management of the building 7. Also, these physical assets must be managed throughout the lifecycle, covering processes such as design, construction, operation, maintenance and the replacement of assets and infrastructure to maximize their value. These efforts ensure better performance, reduced costs, extended useful life and improved return on the investment of the organization’s assets 8.
It has also considered the evolution of a North American origin discipline, called Facility Management (FM), that particularly advocates for a management model of companies' infrastructure that aim to adapt them permanently to the organization and the companies’ personnel at the lowest possible cost, by integrating all the management responsibilities on those resources. With the integration of all the management responsibilities of these resources, this discipline has been focused on physical asset management. The infrastructure has become more complex with the passing of days and contains more technology, sparking major competitiveness with regards to cost, demand, health expectations, consumers’ safety and welfare - in addition to the regard on the impact on the environment 6. Considering that as institutions add new responsibilities and challenges in their work environments to the social purpose of the organization. FM has a very wide scope of work, also aligned with the strategic plan and the organization’s physical assets 9.
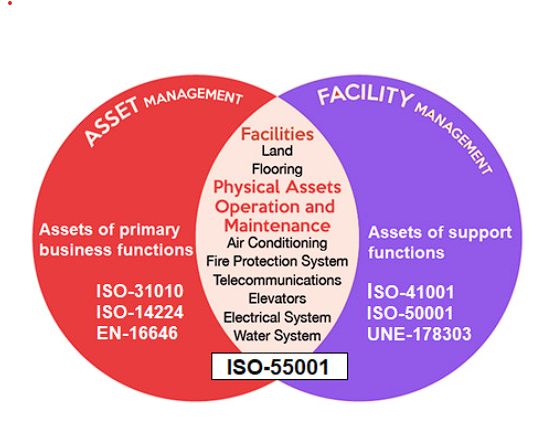
With AM & FM the HI embrace the physical environment, technology, and the risk management that are entailed by the delivery of health services like shown Figure 1. Moreover, this management must be based on the standards of the obligatory system of the guarantee of quality in the health system for maintenance of equipment, the IT, and specially the facilities. Accordingly, HI must determine management objectives, strategies and policies that include physical resources, security maintenance, and adequate preparation for emergencies and disasters. In order to achieve a suitable hospital infrastructure management, its operation must be guaranteed for the service provision, proposing strategies for its continuous improvement, through a safe operation framed within risk mitigation plans. Concurrently, the state regulations must be complied by means: preparing preventive and corrective maintenance plans, physical plant reorganization programs, emergency and disaster plans, assessment of the environmental conditions in critical areas, permanent assessment of infrastructure risk factors, as well as a consideration of every single risk resulting from the health service activity offered by the HI.
This scenario seems to be conducive to the disciplines exposed, since the HI turns out to be autonomous organizations with different management patterns. Although, some authors and organizations 10,11,12,13 emphasized that AM seeks to maximize the value of the organization's assets, but it does not focus on the asset itself, but on the value that it brings to the organization (core business). While the FM organizes the demands of the different groups linked to the company and the relationship of this support with the business activity, to cover the requirements that may arise (non-core business). These disciplines are intertwined in the facilities where maintenance actions have usually been carried out, showing that the infrastructure is a main linkage that allows the organization to develop its main activity.
Therefore, the authors of this work understand that a discipline such as FM, standardized and supported by international regulations, can control the broad spectrum of support activities and services in the health sector. Likewise, the authors have identified is a visible lack of integrated systems with appropriate tools that enable objective decisions to manage the hospital infrastructure adequately.
All organizations are subject to a variety of measurements, particularly in the health sector, since they play a crucial role in the citizens’ well-being. There are different types of HI (public, private, mixed and charitable institutions) that attempt to combine business continuity planning with providing an efficient health service over time. Evidently, there is a need to control the state and performance of the infrastructure results, in the development of specific tools or indicators that can be classified into different categories 14. Mainly in a complex workspace requires special controls adapted to its needs, as well as the monitoring of the overall building performance 4. These HIs are known that in this business you can only objectively improve what can be measured. Therefore, any asset maintenance of a facility management department that faces a process of continuous and rigorous improvement must study the present situation of the organization. Besides, the FM department must propose new measures that aim to align the infrastructure management to the organizational goals, objectives, strategies, and policies.
For this purpose, the authors of this work have explored many definitions and have arrived to Performance Indicators (PI) represent: “a set of quantifiable measures that an industry or service organization uses to measure or compare performance in terms of meeting its own strategic objectives and operations. The PI can vary across organizations and industry sectors, depending on their priorities or criteria.” The use of PI in an FM environment can generate many advantages: they can focus managerial efforts on relatively important performance areas, they can be incorporated into contract specifications and in the documentation used in the selection of the contractors 15. Moreover, management control and accountability will also be reinforced by early intervention and possible corrective measures in response to more visible variations in performance. Because an unsuitable PI management could result in an inadequate infrastructure to support the HI’s operation 16. Just as an excessive infrastructure does not contribute to the organization’s mission, it has cost inefficiencies, inadequacies, and an infrastructure with an unavailability for future needs. Conversely, an appropriate FM approach can provide the necessary support to the organization’s mission, the realization of future facility requirements, greater cost efficiency and the ability to anticipate the results of current management decisions.
The importance of this research is based on the relationship between biomedical technology management and FM throughout the life cycle of the assets in health institutions. This is because FM’s performance evaluation is carried out through soft technologies (PI), and this is aligned with the international state of clinical engineering 17. The purpose of this work has been to develop a brief and relevant list of PI, as well as the classification of them in different categories. This study attempts to support the performance measurement of those key aspects that play a vital role in the physical asset management of the HI, through disciplines such as FM, related to the infrastructure’s lifecycle. This could allow health organizations to comprehensively evaluate the performance in managing your infrastructure using FM’s PI.
Materials and methods
This research has used a model of identification of performance indicators developed by the authors of this study, based on the first three phases of several technological management processes developed by Gregory 18, Fundación COTEC 19, Hidalgo 20, Hidalgo, León & Pavón 21, Amador & Márquez 22 and FPNTI 23. The objective of this model of technological management is to identify, select and adapt the indicators for hospital infrastructure management for the FM discipline, which coincides with the three first points of the models of the named authors.
In a first stage, active monitoring was carried out on the general aspects related to FM and PI; as well as data filtering as part of technological surveillance. Based on these findings, the authors narrowed down the results and extended the bibliographic search in specialized academic search engines (Scopus, Web of Science, and Google Schoolar). The documents found are mostly research papers published in indexed journals and conference papers specializing in diverse topics of FM and PI. After a thorough document gathering and a subsequent information analysis, the authors have made a deep reading of papers to extract information about performance indicators related to the theme in the health setting.
Later in the second stage followed a comparative analysis through the selection and extraction of the most pertinent documents, which had to present enough information on PI applied in infrastructure management and be related to the FM discipline. The specification in the classification of PI was also considered, having a greater affinity with documents related to the health sector. The comparative analysis was completed using a spreadsheet, naming the authors; the country; the date; the relation (or not) with FM; the number of categories of PI; category specification; the number of PI; PI specification and finally, the realization of a list of PI. In the beginning of the third stage, only 21 of 26 papers were left from the initial technological surveillance most of them related to the health sector. Thus, in this last phase, the appointment of the new classifications was initiated and the most relevant PI, connected to these new categories were also compiled.
In this way, the new categories were labeled following a common denominator or the classifications already existing in the documents of technological surveillance. In some cases, the names were partially modified to make them appropriate to the health sector nomenclature. The authors decided to select a maximum of 10 PI among the eligible options that appeared in the resulting documents. These PI were selected by affinity to the identified categories and the evaluation of the most appropriate ones was by reiterating them within the group of documents, if they were measurable or specified. Later, 7 different tables are shown that represent the selected categories to insert the 70 selected PI of the documents examined come from different authors of international relevance in the discipline of FM and in the health setting.
Results and discusión
In the three stages of the technology management process, the authors performed the exploration and identification of several PIs in the 28 documents 4,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50. Afterward, the identified PI were selected and analyzed. Subsequently, the acquisition and adaptation of the PI that met the requirements indicated in the methodology of this work were carried out and were classified into the following 7 different categories:
Financial: The connection between figures collected from financial statements and accounting reports.
Physical: The relationship among the data gathered from behaviors and facilities performance.
Security: The correlation between the data amassed from different behaviors to ensure the security of employees, patients and users of the facilities.
Functional: The junction among the data compiled from different behaviors and the facilities’ functional performance in terms of usefulness, availability, and reliability.
User Experience: The link between the data stored mostly through a series of satisfaction surveys addressed to patients, users and employees regarding the health facilities.
Environmental: The correlation among the data collected from environmental behaviors and practices considering the environmental impact of the facilities management.
Managerial: The relationship between figures and data collected considering the organizational performance, addressed to the facilities management.
In the next tables, the authors show 10 PI in each category related to the diverse areas of the FM that add value to the organization. Moreover, in the tables are established some details such as the name of the PI, acronym of the PI and the objective to this PI for the top management. For example, Table 1 shows the financial performance indicators, which contain major information about the organization’s financial and accounting situation in terms of its infrastructure.
Table 1 Financial PI.
| Nº | Description | Objective |
|---|---|---|
| 1 | Annual Maintenance Expenditure (AME) | Minimize |
| 2 | Maintenance Expenditure per Area (MEA) | Minimize |
| 3 | Building Maintenance Cost (BMC) | Minimize |
| 4 | Maintenance Efficiency Indicator (MEI) | Maximize |
| 5 | Replacement Efficiency Index (REI) | Minimize |
| 6 | Cost Recurrent Value (CRV) | Minimize |
| 7 | Balanced Income and Waste Cost (IWC) | Minimize |
| 8 | Facilities Management Cost (FMC) | Minimize |
| 9 | Average Cost per Bed (ACB) | Minimize |
| 10 | Deferred Maintenance Backlog (DMB) | Minimize |
Source: Authors
The physical performance indicators, presented in Table 2, are linked to the physical performance of the organization’s infrastructure. These indicators provide information on the organization’s infrastructure in terms of size, age, occupation, etc.
Table 2 Physical PI.
| Nº | Description | Objective |
|---|---|---|
| 1 | Building Performance Index (BPI) | Maximize |
| 2 | Building Physical Condition (BPC) | Maximize |
| 3 | Facility Condition Index (FCI) | Maximize |
| 4 | Site and Location (SL) | Maximize |
| 5 | Infrastructure in Satisfactory Condition (ISC) | Maximize |
| 6 | Building Average Age (BAA) | Minimize |
| 7 | Thermal Comfort (TC) | Maximize |
| 8 | Area per Employee & Bed (AEB) | Minimize |
| 9 | Properties and Real Estate (PRE) | Maximize |
| 10 | Occupancy of Hospital Assets (OHA) | Maximize |
Source: Authors
Table 3 shows the safety performance indicators that connect the users, patients, and employees with the organization. These indicators can be analyzed using the perception of the agents or employees concerning their conditions and the risk presented within the healthcare service.
Table 3 Safety PI.
| Nº | Description | Objective |
|---|---|---|
| 1 | Percentage Compliance from Statutory (PCS) | Maximize |
| 2 | Risk Prevention Management (RPM) | Maximize |
| 3 | Risk Adjusted Backlog Maintenance (RBM) | Minimize |
| 4 | Maintenance Related to Incidents and Accidents (MIA) | Minimize |
| 5 | Number of Solved Safety Non-Conformances (NSN) | Minimize |
| 6 | Lost Time Due to Non-Fatal Accidents (LTA) | Minimize |
| 7 | Number of Fire Incidents (NFI) | Minimize |
| 8 | Satisfactory Working Conditions (SWC) | Maximize |
| 9 | Provision of Safe Environment (PSE) | Maximize |
| 10 | Employees Perception of Risk Prevention Management (EPR) | Maximize |
Source: Authors
The functional performance indicators, shown in the Table 4, provide a view of the functionality of the infrastructure, considering the occupation, cleanliness, and adequacy of the workspace. These indicators offer information about the space used by the organization to carry out its main activity.
Table 4 Functional PI.
| Nº | Description | Objective |
|---|---|---|
| 1 | Functional Index (FI) | Maximize |
| 2 | Patient Density Coefficient (PDC) | Maximize |
| 3 | Bed Availability Index (BAI) | Maximize |
| 4 | Space Utilization Index (SUI) | Maximize |
| 5 | Ability to Comply Requirements (ACR) | Maximize |
| 6 | Infrastructure Reliability (IR) | Maximize |
| 7 | Quality of Scheduling (QS) | Maximize |
| 8 | Service Inactivity Time (SIT) | Minimize |
| 9 | Mean Wait Time (MWT) | Maximize |
| 10 | Cleaning Effectiveness (CE) | Maximize |
Source: Authors
Table 5 presents a set of user experience performance indicators linked to the results obtained from patients, users and employees’ surveys. Usually, these enquiries regarding their experience within the healthcare infrastructure are designed to support the improvement of activities to achieve the organization’s goals for users’, patients’ and employees’ experience.
Table 5 User Experience PI.
| Nº | Description | Objective |
|---|---|---|
| 1 | Building Occupant Satisfaction (BOS) | Maximize |
| 2 | Community Satisfaction and Participation (CSP) | Maximize |
| 3 | Privacy and Dignity (PD) | Maximize |
| 4 | Cleanness and Tidiness (CT) | Maximize |
| 5 | Food Services (FS) | Maximize |
| 6 | Hospital Environment (HE) | Maximize |
| 7 | Respect the Values, Preferences and Needs (VPN) | Maximize |
| 8 | Friends and Family Test (FFT) | Maximize |
| 9 | Number of Complaints (NC) | Minimize |
| 10 | Sustainability Urban Mobility (SUM) | Maximize |
Source: Authors
The environmental performance indicators outlined in Table 6 present the organization’s environmental impact. These indicators cover the use of resources, energy, the quality of the environment, the level of pollution, recycling and the impact of the sustainability of the organization.
Table 6 Environmental PI.
| Nº | Description | Objective |
|---|---|---|
| 1 | Sustainability Index (SI) | Maximize |
| 2 | Environment Cost (ENC) | Minimize |
| 3 | Energy Consumption (EC) | Minimize |
| 4 | Water Consumption (WC) | Minimize |
| 5 | Wastewater Indicator (WSI) | Maximize |
| 6 | Carbon Dioxide Emissions Indicator (CO2) | Minimize |
| 7 | Daylighting in Building Index (DLB) | Maximize |
| 8 | Hazardous Operational Waste (HOW) | Minimize |
| 9 | Energy Saved with Conservation & Efficiency (ES) | Maximize |
| 10 | Air Quality Compliance (ACQ) | Maximize |
Source: Authors
The managerial performance indicators based on the top management practices in relation to the infrastructure are listed in the Table 7. These indicators detail the management of staff, their competence, effectiveness and their compliance with the organization’s goals, strategy, and responsiveness to problems.
Table 7 Managerial PI.
| Nº | Description | Objective |
|---|---|---|
| 1 | Managerial Span of Control (MSC) | Maximize |
| 2 | Training Days per FM Staff vs Incentives (TDI) | Maximize |
| 3 | Lost Time Frequency Rate - for FM Staff & Contractors (LTF) | Maximize |
| 4 | Competence of Staff (CS) | Maximize |
| 5 | Effectiveness of FM’s Information (EFI) | Maximize |
| 6 | FM Organizational Capacity (OC) | Maximize |
| 7 | Alignment of FM Strategy with Organization Strategy (ASO) | Maximize |
| 8 | Compliance with Provisions of Service Level Agreements (SLA) | Maximize |
| 9 | Compliance of Property Asset Management Strategy (AMS) | Maximize |
| 10 | General Management Costs vs Direct Costs of Services (GMC) | Minimize |
Source: Authors
Considering the results obtained in this technological surveillance, the authors of this work appreciate that many of these results had disparities both in the classification of the categories, in the number of PI, and in their specification. This disparity in results may have caused the lack of compilation studies like this work, especially those that cover different categories. Considering the results obtained in this technological surveillance, the authors of this work appreciate that many of these results had disparities both in the classification of the categories, in the number of PI, and in their specification. This disparity in results may have caused the lack of compilation studies like this work, especially those that cover different categories. However, in this study more recent works have been found 40,42,44,45,46,47,48,49,50 who have classified many PI (up to 61) into more categories than other authors who used to do so in the classic categories (financial, physical, functional and user satisfaction). This has confirmed that our study is in line with being able to classify PI for FM into these seven categories that represent a large part of the functions of FMers. For this, the purpose of this study has not been modified, as the results of this work can contribute to an appropriate use of performance indicators in facility management and continue to cover the publication of new research in the health sector.
The authors have identified the need to consult some FM worldwide experts to verify the efficacy of these PI in the actual practice of this discipline in the health sector. This could imply the development of a new research line in a clinical/hospital engineering. In addition, it’s vital to show later these indicators to maintenance management experts, considering that current maintenance or infrastructure managers share an important number of functions with facility managers (FMer). With the analysis of the work done by the authors up until now and taking the aforesaid steps, a list of effective PI could be created to manage hospital infrastructure following an FM-based discipline. Therefore, HI could adapt these PI to their vision, mission, and organizational policies, considering that proposed lists and the resultant performance indicators of future studies do not form a definitive record of PI that HI must be mandated to use in the future. Quite the opposite, FMer can apply those indicators that they find useful, adapt others, and including combine some of them.
This study proposes to select, adopt, or develop those FM performance indicators that are conducive to the efficient physical asset management of a HI supervised by the FMer or by those who perform their functions. It should be added that these indicators could be efficient tools during hospital infrastructure management, to record the present, past and future information that has previously divided its management. It should be remembered that the application of new information technologies enables a greater volume of data related to the organization management to be treated, though it causes high levels of data saturation among the organization’s managers. Therefore, in view of this situation, the authors have been working on the selection of FM performance indicators to attempt to simplify and optimize hospitals’ management of assets through this discipline. In this regard, FM can yield new possibilities to a wide range of supporting activities within the organization, such as preventive maintenance, drawing on other technologies such as big data, etc.
According to the proposed PI lists, the authors believe that the use of these lists is a similar way to elaborate on the “one-page management reports” for each of the categories so that the personnel in charge of management can have as much information as possible with the least amount of data 51. Still drawing on the PI of FM, the authors would argue that these and other indicators are effective instruments for Service Level Agreements (SLA) between clients and providers: these agreements determine the minimum, expected, and agreed quality of a service rendered to a client. Because the performance indicators measure the efficiency of the desired operation and the organization’s objectives so it’s therefore important to quantify those indicators and the service compliance, with the intention of fulfilling promises and improving service quality. There are many variables that cause SLA changes within the same service and for different customers however, the PI are the same for that service.
The authors of this work assert that the results of this study are aligned with the research of Torres & Escobar 17, whose work has investigated the key points that aim to better technology management in the healthcare sector. Because according to the above, other authors 52,53,54,55,56 among others have promoted the use of Key Performance Indicators (KPI) in different sectors: education, transport, services, etcetera. However, of these researches it can be deduced that PI (or KPI, in those investigations) are necessary to measure performance, which in turn yields a substantial feedback loop for strategic change.
In addition, the authors of this study hold that the proper use of PI also can contribute to the fulfillment of the accreditation of the facility management system; and consequently, any hospital could get any kind of accreditation such as the Joint Commission International. In order to obtain this accreditation, one of the greatest challenges for some HI in developing countries is to achieve the standards of services offered in high-quality hospitals in developed countries. Similarly, the outcomes of this study have not yet developed those checked indicators that align HI physical asset management with the organization’s goals, objectives, strategies, and policies. Above all, because most of the documents reviewed for this work did not offer this information either. However, this work opens the doors to investigate more about the use of FM performance indicators in health institutions and the alignment of the proposed PIs with current uses by FMer.
Generally, the HI (including those institutions outside Anglo-Saxon trends) have a maintenance program documented into their internal functioning procedures, although this does not prove that they are fulfilling the organization’s objectives, strategies and policies. This carries us lead to reflection on an international state of clinical engineering (and now FM state too) for the identification of strengths/weaknesses of key aspects of the development of the physical asset management in Latin America 17. Also, the Anglo-Saxon trends review in the health sector of disciplines such as FM and its alignment with the development of international standards in recent years (EN-15221 and ISO-41000) with the use of IP for proper management of the infrastructure.
Conclusión
The achievement of this study has been a preliminary proposal of dimensions and PI of FM with a high theoretical level. Hence, the authors expect it necessary for later studies to validate these results with the help of international FM experts and with practical assessment by hospital physical asset managers. The authors of this study recommend that in the future validation process, several case studies should be conducted in some HI to verify the utility of these PI of FM. Above all, because most of the HI worldwide (especially in countries outside the Anglo-Saxon trends) have not yet implemented FM in the healthcare setting.
The objective achieved in this work has been to identify several indicators and dimensions of FM, through a bibliometric study, that allow FMers to create a system of indicators to obtain more concise and complete reports. These findings may demonstrate the alignment of the different areas to the goals, objectives, strategies, and organizational policies of HI. Because there are studies that determine that PI lead to optimized infrastructure management. However, the inadequate application of these dimensions, indicators of FM and the lack of a holistic approach within the HI could generate a low performance in the application of this tool. With this work, the authors intend to shed light on the use of these indicators to achieve operational excellence in healthcare physical asset management. In fact, this research may be the beginning of a new topic linked to the research line of hospital engineering, that deals with FM based on performance indicators.
Considering the perspective of this study, further to the preliminary proposal of dimensions and performance indicators selected by the authors in this work, other indicators exist that are not mentioned in the document. These PI could have been developed and used by any organization for the search the effectiveness of the administration of its physical assets with respect to the objectives, strategies, and organizational policies. In addition, this system of indicators could be beneficial when carrying out and controlling SLA contracts with FM service providers, in any of their areas (in-house or outsourcing). This issue must be developed in upcoming studies to strengthen the connection of PI and the control of SLA contracts between service contracting parties.
In short, this work has been centered in the phrase attributed to Edward Deming "you cannot improve what is not controlled; you cannot control what is not measured; you can't measure what you don't define". Hence, the FMer must be able to apply common sense to the data they obtain in their work because measuring something does not make it manageable. The possibility of measuring something really makes it quantifiable, which is already an important contribution to the management of facilities. Also, this work has pretended identifies key aspects that HI need to improve, such as: training for technical and health personnel, maintenance scheduling, technology evaluation in all aspects, strategic planning, assessment of needs, totaling the cost of assets, risk management, repairs, investigation of incidents, service agreements, and documented information, among others.