INTRODUCTION
Coronary artery disease (CAD) is characterized by a deposit of lipids in cells lining the wall of an artery, obstructing the blood flow to the heart (Bonow, Mann, Zipes, & Libby, 2013). The clinical manifestations of CAD involve myocardial ischemia, acute myocardial infarction (AMI), congestive heart failure and sudden death (Magalhães et al., 2015). The risk factors for CAD are family history, obesity, sedentarism, diabetes, hypertension, smoking, and psychosocial factors, such as symptoms of anxiety and depression (Bonow et al., 2013; Timerman, Ferreira, & Bertolami, 2012).
One of the treatments for CAD is percutaneous coronary intervention (PCI), which includes the balloon angioplasty, the implantation of the intracoronary stents and other interventions with the use of catheters. An inflated balloon is used inside the occluded coronary artery, which compresses the atherosclerotic plaque against the vessel wall, thus allowing clearance and use of stents, consisting of small prostheses with the shape of a tube, expandable, to reduce the blockage or narrowing of the artery. The coronary stents are divided into two categories: non-pharmacological and pharmacological (Levine et al., 2011; Mattos et al., 2008). The choice of treatment will depend on the stage and the severity manifested by the pathology (Centemero, 2014).
The symptoms of anxiety are related to the development of cardiac events in the general population. A meta-analysis study concluded that anxiety is considered a risk factor for cardiac patients, being associated with adverse cardiac events, new cardiac events and causes of mortality (Roest,
Martens, Jonge, & Denollet, 2010). Depressive symptoms are also related to certain hearth diseases, and may be considered as a cause, risk factor or consequence of them (May et al., 2009; Sardinha, Araujo, Silva, & Nardi, 2011).
Even though the psychological symptoms could be frequent and have a serious impact on patients' lives, often they pass unnoticed (Ceccarini, Manzoni, & Castelnuovo, 2014; Huffman, Celano, & Januzzi, 2010). In addition to presenting higher rates of morbidity and mortality in the long term, if these symptoms are not treated, both quality of life and the outcome of the disease can be impaired (Jeenger, Wadhwa, & Mathur, 2014).
The objective of the present study was to describe the socio-demographic profile, cardiac diagnosis, risk factors and aspects related to the mental health of adult and elderly patients hospitalized after PCI and to analyze the relationship of these parameters with the intensity of anxious and depressive symptoms in these patients.
METHOD
Delineation
This is a cross-sectional, analytical study, of correlational and comparative nature (Volpato, 2017).
Participants
266 adult and elderly patients who had undergone PCI participated in the study. All patients, aged 50 years old or more, who did not present dementia diagnosis, were literate, had been subjected to PCI and were hospitalized, were included. Patients who presented a dementia diagnosis or visual impairment that hindered filling out the instruments, and patients who did not know how to read and write were excluded. The confirmation of extreme dementia diagnosis occurred in advance, through the consultation of medical records.
The sample was stratified by sex (male and female) and age (50 to 59 years old; 60 years old or more). It was selected out of a population of 793 patients, according to data from 2014 described in the DATASUS (Brazil, 2015), with a sampling error of 5% and a confidence interval of 95%. The minimum sample size determined was 266 patients who were subjected to PCI and distributed as follows: a) 183 men (46 of them aged between 50 and 59 years old and 137 aged 60 years old or more) and 83 women (16 of them aged between 50 and 59 years old and 67 aged 60 years old or more).
The average age was 64.5 years old (SD = 8.9 years old). Most patients were males (68%), had elementary school education (80.1%), were married (79.7%), lived with someone else (89.1%) and had children (94.4%). The cardiac diagnosis for the majority of patients was AMI (64.3%); most of them also had a family history of heart disease (62.8%) and had undergone angioplasty with stent placement (95.1%), by the National Health System (NHS) (97.7%). The average time of diagnosis was of 1680.8 days (SD = 2429.3 days).
Instruments
A questionnaire was constructed for this study with the objective of collecting information related to socio-demographic data, cardiac diagnosis, risk factors and data concerning the mental health of patients hospitalized after PCI.
The Beck Anxiety Inventory (BAI) consists of a scale of 21 symptoms, whose objective is to assess the intensity of anxiety symptoms. Cunha validated the instrument for the Brazilian population in 2001. The scale measures the following symptoms: numbness or tingling; heat sensation; tremors in the legs; inability to relax; fear that the worst might happen; dizziness; palpitations or heart acceleration; imbalance; fearfulness; nervousness; suffocation sensation, shaky hands; tremors; fear of losing control; fear of dying; shortness of breath,; dread, indigestion or discomfort in the abdomen; fainting sensation; burning face; sweat (not because of heat). The assessment is performed with a 4 points Likert scale (0-3), where the maximum score is 63 points. As a result, the minimum level of anxiety corresponds to a score ranging from 0-10; mild level, from 11-19; moderate, from 20-30 and severe, from 31-63. In studies for validation with the Brazilian population, the instrument presented a Cronbach's alpha precision index ranging from 0.83 to 0.92 for non-clinical samples and from .75 to .92 for a medical-clinical sample (Cunha, 2001).
The Beck Depression Inventory - Second Edition (BDI-II) is a scale with 21 items, including symptoms and behaviors related to depression. It was validated for Brazil by Gorenstein, Pang, Argimon and Werlang in 2011. The assessed items on the scale are: sadness, pessimism, past failure, loss of pleasure, sense of guilt, sense of punishment, self -esteem, self-criticism, suicidal thoughts or desires, crying, agitation, loss of interest, indecision, devaluation, lack of energy, changes in the sleep pattern, irritability, changes in appetite, difficulty in concentrating, tiredness or fatigue, loss of interest in sex. The scale items allow the assessment of increasing severity of depression. The assessment is carried out with a 4 points (0-3) Likert scale, where the maximum score is 63 points, and items 16 and 18 have seven response options to assess the increase and decrease of behavior. The total score indicates the severity of depression in terms of minimum (a score from 0 to13), mild (14-19), moderate (20-28) and severe (29-63) (Gorenstein, Pang, Argimon, & Werlang, 2011).In a validation study in Brazil, the BDI-II presented a Cronbach's alpha precision index of .93 in a non-clinical sample (Gomes-Oliveira, Gorenstein, Lotufo Neto, Andrade, & Wang, 2012).
Procedure
The data collection took place in the hemodynamic sector of a hospital located in southern Brazil, within the period of May to October 2016. In the shift after they have performed the PCI, the researcher went to the location and presented the research objectives to the patients whose profile corresponded with the study's inclusion criteria, and invited them to participate in it. All the patients signed the Informed Consent Form, according to resolution 466/12 of the National Health Council. In the free and clarified consent form, it was stated that the study did not involve any risk to the physical health of patients but that filling out the instruments could generate some emotional discomfort. If this occurred, the application of the instrument would be suspended by the researcher.
The questionnaire was completed by the researcher, and the BAI and the BDI-II, by the patients, in an estimated period of approximately 30 minutes. The Research Ethics Committee of the University of Passo Fundo/RS, report 1.389.673, approved the research.
Data analysis
To analyze the collected data, the Chi-Square Test, Kolmogorov-Smirnov Test and ANOVA were used. The level of significance was p < .05.
The Chi-Square Test was applied to analyze the comparison of sociodemographic data, cardiac diagnosis, risk factors and data related to the intensity of the symptoms of anxiety and depression. The Kolmogorov-Smirnov Test was used to analyze normality. With respect to the ANOVA's analysis, it was applied to compare the average age at the time of cardiac diagnosis, considering the amount of times per week that the patient performed physical activity, the amount of cigarettes that he smoked per week, the time elapsed since he stopped smoking, the amount of alcohol consumption, the time elapsed since the previous diagnosis of anxiety and depressive disorder, as well as the dosage of psychiatric medication prescribed according to the intensity of the symptoms of anxiety and depression.
RESULTS
The following results will be presented regarding the risk factors, aspects related to mental health and the intensity of anxiety and depression symptoms of hospitalized patients after percutaneous coronary intervention. Also, the relationship between the intensity of anxiety and depression with socio-demographic data, risk factors and aspects related to the mental health of these patients is shown.
In terms of risk factors, the majority was composed by hypertensive subjects (83.5%) that presented dyslipidemia (51.5%), but who did not have diabetes (61.7%) or obesity (81.6%). The majority (69.9%) performed physical activity, with an average of 4.08 (SD = 2.16) times per week. Regarding tobacco consumption, the majority were ex-smokers (44.7%); the average of smoked cigarettes per week in smokers was 135.4 (SD = 117.9) and the average of ex-smokers in relation to the time elapsed since the date when they stopped smoking was 54.299.6 (SD = 4.786.5) months. Concerning alcohol consumption, the majority of patients did not use it (80.8%), and among those who did, most of them consumed beer (12%), being the average ingestion 1.3L (SD = 1.3) per week.
The assessment of prior diagnostic of anxiety and depressive disorder was done by self-report. The majority did not provide diagnosis of anxiety disorder before the PCI (95.1%), and none of them had had a previous diagnosis of depressive disorder (81.2%). Among those who had a previous diagnosis of anxiety disorder, the average time of diagnosis was 128.9 months (SD = 139.8) and of depressive disorder was 327.3 months (SD = 1.449.1). The majority did not receive psychological treatment (99.6%), and did not take psychiatric medication (78.9%). The category of anxiolytics appeared more frequently in those who used psychotropic drugs (62.5%).
Regarding the quantitative variables, the Kolmogorov-Smirnov test showed no rejection, according to Table 1.
Most patients presented symptoms of anxiety at a severe level (29.7%) and depressive symptoms of minimum intensity (51.9%), as shown in Table 2.
The average age of the patients with symptoms of anxiety at a minimum level was 66.61 (SD =9.42), at mild level was 65.17 (SD= 8.97), at moderate level was 62.00 (SD= 8.18) and at severe level was of 63.89 (SD=8.52) years old. A significant difference in terms of the average age among the minimum and moderate symptoms of anxiety (p =.026) was found with the use of ANOVA, as described in Table 3.
Table 3 Relationship between level of anxiety symptoms and average age

Note: ANOVA (F = 3.131); Tukey Test. The averages are shown for the groups in homogeneous subsets. The sample size was used to define the harmonic average (Average age = 65.43), since the group sizes were unequal.
The relationship between the socio-demographic data and the level of anxiety symptoms were evaluated through the Chi-Square Test. There was a significant difference for sex (p < .001), i.e., women showed a level of severe anxiety. No significant difference was found for schooling (p = .685), marital status (p = .094), living with somebody (p = .217), and having children (p = .111). There was no significant difference for the cardiac diagnosis (p = .611) and the procedure performed (p = .946).
In the calculation that related risk factors with intensity levels of anxiety symptoms, by means of the Chi-Square Test, there was a significant difference with respect to family history (p = .011), as shown in Table 4.
Referring to aspects related to mental health, the Chi-Square Test showed a significant difference in the previous diagnosis of depressive disorder (p = .011). No significant difference was found for prior diagnosis of anxiety disorder (p = .550), use of psychotropic drugs (p = .663) and type of medication (p = .738).
Table 4 Level of anxiety symptoms and risk factors present in hospitalized patients in post-PCI

Note. Values in brackets represent the percentages; the Chi-Squared Test; significant value forp < .05.
The ANOVA Test did not show a significant difference regarding time elapsed since diagnosis (p = .888), the amount of times per week that the patient performs physical activity (p = .899), the number of cigarettes that he smokes per week (p = .165), the time elapsed since quitting tobacco (p = .378), the amount of alcohol consumption (p = .162), the time elapsed since the diagnosis of anxiety disorder (p = .685), the time elapsed since the diagnosis of depressive disorder (p = .752) and about the medication dosage (p = .624).
Regarding the intensity of depressive symptoms and average age, the ANOVA Test showed that there was no significant difference (p = .070), as shown in Table 5.
Table 5 Relationship between intensity of depressive symptoms and average age
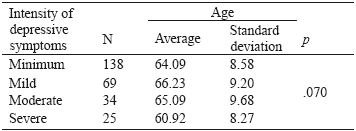
Note. ANOVA (F = 3.131); Tukey Test. The averages are shown for the groups in homogeneous subsets. The sample size was used to define the harmonic average (Average age = 43.88), since the sizes of the groups were unequal.
In respect to gender, women showed more depressive symptoms of severe intensity (p < .001). There was no significant difference in schooling (p = .369), marital status (p = .234), living with somebody (p = .136) and having children (p = .908).
In the calculation that related risk factors with intensity of depressive symptoms, using the Chi-Square Test, no considerable differences were found, as shown in Table 6.
Table 6 Intensity of depressive symptoms in terms of risk factors for hospitalized patients in post-PCI

Note: Values in brackets represent the percentages; the Chi-Squared Test; significant value for ap < .05.
Regarding mental health issues, the Chi-Squared Test showed no significant difference for the previous diagnosis of anxiety disorder (p = .081). With respect to the previous diagnosis of depressive disorder, there was a significant difference (p = .001). There was no difference for use of psychiatric medication (p = .086) and type of medication (p = .367).
The ANOVA Test did not show a significant difference in terms of the time elapsed since the cardiac diagnosis (p = .430), or about how often the patient performed physical activity (p = .644), the amount of cigarettes he smoked per week (p = .611), the time elapsed since quitting tobacco, (p = .401), the amount of alcohol consumption (p = .950), time elapsed since the diagnosis of anxiety disorder (p =.870), time elapsed since the diagnosis of depressive disorder (p = .166) and the medication dosage (p = .504).
DISCUSSION
The patients' demographic profile found in this study corroborates the data from other studies. A similar study was carried out in a U.S.A. hospital, where 70% of the patients were men, with an average age of 62 years old (Watkins et al., 2013). Another study in the Netherlands also found that 76.9% were men, with an average age of 63.3 years old (Damen et al., 2013). Data relating to marital status agree with the results of a study conducted in Brazil, where most participants of the sample were married or living in a stable union (Furuya et al., 2013). In terms of schooling, a survey conducted in Brazil showed that 44% of the patients had completed elementary school (Schmidt et al., 2011). It is estimated that NHS is responsible for 80% of PCIs carried out in Brazil (Piegas & Haddad, 2011).
Regarding the procedure, the data corroborate a study conducted in India, in which 90% of the patients did the angioplasty with stent placement (Chaudhury & Srivastava, 2013), and in another study, 100% also implanted stent (Schmidt et al., 2011). In respect of the diagnosis, in a study carried out in Portugal, the majority had a diagnosis of AMI (58.8%) (Pacheco & Santos, 2015), and it was found that PCI reduces mortality and ischemic events and improves quality of life (Blankenship et al., 2013).
As far as risk factors are concerned, the findings coincide with the conclusions of a research carried out with patients after PCI in Brazil, of which 100% were hypertensive and 93.8% had dyslipidemia (Richter et al., 2015). In a study conducted in Iran, 36.8% were hypertensive and 21.4% were diabetic (Hosseini, Ghaemian, Mehdizadeh, & Ashraf, 2014). In a research that aimed to determine the prevalence of risk factors for DAC in cities of southern Brazil, dyslipidemia was found in 43% and hypertension in 40% of patients (Gus et al., 2015). In this study, the majority of patients performed physical activity; they were ex-smokers and did not use alcohol. In other findings, the majority did not smoke cigarettes (47.5%) (Chaudhury & Srivastava, 2013) and also did not consume alcoholic beverages (55.6%) (Pacheco & Santos, 2015).
In this research, most patients had no previous diagnosis of anxiety disorder and depressive disorder, they didn't use psychiatric medication and did not received psychological treatment. The data are in agreement with another study, which showed that 76% of the patients had never received psychiatric treatment, 31% reported making use of psychotropic drugs and 12% had a previous diagnosis of depressive disorder (Schmidt et al., 2011). The literature highlights that the psychological treatment for cardiac patients reduces symptoms of anxiety and depression, pain and, therefore, improves the quality of life (Chaudhury & Srivastava, 2013; Ski, Jelinek, Jackson, Murphy, & Thompson, 2016). When the patient presents psychological symptoms that primarily compromise adherence to clinical treatment, a referral to psychotherapy is necessary (Jeenger et al., 2014).
In this study, the majority of patients presented symptoms of anxiety at a severe level and depression with a minimum intensity. The findings confirm the information from a research that showed symptoms of anxiety in 29% of patients and depression in 25%, using the BAI and the Beck Depression Inventory (BDI) (Schmidt et al., 2011). Another study in Brazil that used the Hospital Anxiety and Depression Scale (HADS) as assessment instrument, found that 32.5% of the patients presented symptoms of anxiety and 17.5% of depression (Carvalho et al., 2016). In another research using the same instrument, approximately 20% of the sample presented symptoms of anxiety and depressive disorder clinically significant (Watkins et al., 2013).
A study - which had as instruments the BDI-II and The Self-Rating Anxiety Scale (SAS) - and aimed to verify the prevalence of depression and anxiety in patients in the Czech Republic, identified depressive symptoms in 21.5% of the patients and anxiety symptoms in 8.9% of them after 24 hours of PCI (Kala et al., 2016). The specialized literature points out that patients affected by an AMI have symptoms of anxiety and depression after diagnosis, resulting in a lower probability of resuming their work activities, less tolerance to the practice of physical activity, less adherence to medical treatment, cognitive decline and lower quality of life (Huffman et al., 2010; Mattos et al., 2008; O'Neil, Sanderson, & Oldenburg, 2010). In addition, these symptoms are associated with higher rates of complications, the possibilities of reinfarction and the risk of death (Mastrogiannis et al., 2012; Norlund, Olsson, Burell, Wallin, & Held, 2015).
This study showed that patients with lower age showed a higher level of anxiety symptoms. In another study, there was a correlation between anxiety scores and younger age (p < .001) (Watkins et al., 2013).These findings corroborate a cohort study conducted in Asia, where patients with ages between 45 and 64 years old presented a higher risk of anxiety (Feng et al., 2016). Elderly patients who have already thought of their own death may experience fewer symptoms of anxiety (Zhao, Luo, Wang, & Su, 2008).
The study showed that there was a relationship between anxiety symptoms and a family history of heart disease. The literature points to heredity as a risk factor for CAD (Bonow et al., 2013) and a research confirmed that 50% of the patients had a history of heart disease in the family (Gus et al., 2015). In a study that sought to characterize the profile of patients with symptoms of anxiety in a hospital in Brazil, it was identified that 41.3% of the sample had a family history of VCDs (Bochi, Ribeiro, & Paes, 2014). Similarly, in another finding, 67% of the patients had a family history of this condition (Lucena et al., 2016).
An association was found between anxiety symptoms and previous diagnosis of depressive disorder (p = .011); in other words, patients who had a previous diagnosis of depressive disorder presented symptoms of anxiety at a severe level. Patients diagnosed with depressive disorder have a negative vision of themselves, characterized by pessimistic and hopeless thoughts (Beck, 2013). The patients' beliefs about the disease influence the management of their pathology, revealing ideas, concepts and attitudes about the care and own health (Bonetti, Silva, & Trentini, 2013; Gama, Musi, Pires, & Guimarães, 2012).
In terms of the presence of anxiety symptoms, there was a relationship with sex; in other words, women showed a higher prevalence of these symptoms (p < .001) at a severe level. This supports the results of other studies, which have found a correlation between symptoms of anxiety and female sex (p = .032) (Watkins et al., 2013), and with patients hospitalized in Brazil, where anxiety symptoms were also associated with females (p = .002) (Carvalho et al., 2016). Furthermore, patients who used medication for depression or anxiety had higher scores in the assessment of anxiety (Trotter, Gallagher & Donoghue, 2011).
In the same way, other studies also revealed that women experienced more depressive symptoms than men 24 hours after the PCI (p < .001) (Kala et al., 2016) and depressive symptoms were associated with female sex (p = .022) (Carvalho et al., 2016). Another study found that women had more depressive symptoms (43.7%) when compared to men (14.8%) and the difference between the groups was significant (p < .001) (Furuya et al., 2013). Depressive symptoms in women are related to biological matters, psychosocial aspects (Dessotte et al., 2015) and cultural issues, since women tend to express their feelings more openly, have more freedom to cry and seek expert help from health professionals more frequently than men (Emslie, Ridge, Ziebland, & Hunt, 2007; Fernandes, Nascimento, & Costa, 2010).
Another significant factor has to do with the previous diagnosis of depressive disorder. In other words, patients who already had this diagnosis had the highest score of depressive symptoms of severe intensity (p < .001). It is estimated that individuals with a diagnosis of this pathology have twice the risk of developing CAD (Khawaja, Westermeyer, Gajwani, & Feinstein, 2009). If the patient already had a history of depressive symptoms before the cardiac diagnosis or if there are cases of depression in the family, there will be a higher probability of presenting those symptoms (Blay, Andreoli, Fillenbaum, & Gasta, 2007).
Based on this study, it can be concluded that symptoms of anxiety at a severe level and depressive symptoms of minimum intensity were found in adult and elderly patients who underwent PCI. It was found that younger patients had higher scores of symptoms of anxiety and depression. There was an association between symptoms of anxiety with the female sex, with a family history of heart disease and diagnosed with major depressive disorder before PCI. Depressive symptoms were also related to the female gender, as well as to the previous diagnosis of depressive disorder. Therefore, the importance of assessing psychological symptoms after the intervention, as well as the need for follow-up by a psychology professional in this context is evident.
One of the limitations of this research is the fact that the sample was not compared with individuals who had not been submitted to cardiac intervention. It is suggested that new studies are conducted using a longitudinal design to monitor these patients post-discharged from hospital. Furthermore, psychological intervention studies during hospitalization should be carried out, in order to verify whether there is a decrease of anxiety symptoms.











 text in
text in 




