Introduction
Since 1990, the availability of high quality and low cost drugs has incremented exponentially, and as a result, intravenous consumption of these drugs has increased1. Opiates were among the most used substances in 2013 (71.8%)2, making them a current pressing issue for the Colombian Social Protection Ministry taking into account their impact on public health due to their association with the spread of HIV infection3,4. People who inject drugs (PWID) are seven times more likely to get HIV that the general population5.
It is estimated that there are approximately 6 million intravenous drug consumers around the world5. According to the last heroin consumption report in Colombia, there are around 15,000 PWID in the country, which is a worrying figure since the use of this type of drugs entails a higher risk for the health of the consumer6.
In 2017, a non-governmental Colombia reported 13,310 infected people with HIV highlighting sexual contact as the main transmission mechanism (91.4%). Additionally, they observed other mechanisms like injecting drugs with 0.13% (11 cases)7, which was slightly higher than what was reported in 2015 (eight cases), evidencing the importance of following up with this population.
HIV infection in Colombia has been defined as a concentrated epidemic, which means the disease occurs mainly in high vulnerability groups: sex workers, males who have sex with other males (MSM), and PWID, with prevalences higher tan 5%, while for the rest of the population it is below 1%. This concept was established by the World Health Organization7.
It is important to remember that in PWID, the HIV virus spreads much faster than among the general population8, given the fact that sharing syringes has been reported as a factor which increases the risk of acquiring the virus9. The paraphernalia is also highly important when talking about HIV in PWID10.
The study “Determinants of HIV positivity among injecting drugs users in Delhi and Punjab” evidenced that 10% of this virus transmission can be attributed to the use of injected drugs 11. Additionally, with the implementation of risk decrease policies, such as syringe exchange programs, replacement with methadone, peer educational programs, etc., a reduction in the transmission of the virus has occurred 12. This article aimed to identify associated factors with HIV infection in people who inject drugs in Medellin .
Materials and methods
This was a cross-sectional descriptive study of people who inject drugs, conducted between December 2017 and January 2018, in Medellin, Colombia, using the respondent driven sampling (RDS) methodology13. The sample size was calculated with the formula for 5% HIV prevalence proportion in Colombia, with a 95% confidence interval, a design effect of 1, and 5% precision, for a total of 224 participants.
The procedure used for the collection of the information was through the initial selection of three seeds or non-randomized participants from the target population. This selection was made through key informants, which then chose other PWID that complied with the inclusion criteria: at least 18 years old, active consumers (in the last six months), who had consumed psychoactive substances outdoors in Medellin, and finally, those who accepted through signing an informed consent. From these seeds we started the recruiting waves, until completing 224 subjects.
Two types of incentives were given to the participants: a primary incentive or for participating in the study, and a secondary one, linked to the successful participation of three new subjects (an approximate value of USD $4 and $7, respectively). The size of the target sample was reached after approximately eight weeks.
The instrument included questions, such as demographic characteristics, HIV knowledge, injection practices, sexual practices, and injection networks. Following the guidelines of the Colombian guide for HIV diagnosis, those people whose first test was positive were subjected to a second blood collection on filter paper to perform a confirmation test.
As a bias control measure in the interviewees, we carried out a standardizing training prior to gathering the information. We guaranteed the confidentiality of the information provided by the population.
This project was endorsed by the Ethics Committee of the Universidad CES. For the analysis of the data we used SPSS version 21, Universidad CES licence.
Results
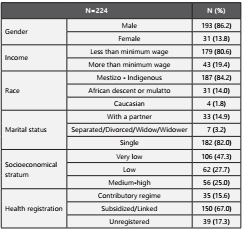
We recruited 224 people who injected intravenous drugs in total (N=224), from which 86.2% were men, 82.0% were single, most of them were mestizo and indigenous (84.2%), and 47.3% came from a very low social status. Similarly, we found that 67.0% belonged to a subsidized or linked health regime (table 1). We observed that HIV prevalence among the consumers in the metropolitan area of Medellin was 3.6%.
Table 1 Sociodemographic characteristics of people who inject drugs in Medellin. December 2017- January 2018.
Among the analyzed factors we found that if the number of friends with whom drugs were consumed before its first injection was around half of them, HIV probability increased 67% (RPc=1.67, 95% CI: 0.184-15.155), compared to when only a few of them consumed drugs. The proportion of users who reported having used syringes used by other people was 37.4%, and they were 1.71 times more likely to present with HIV infection (RPc=1.71, 95% CI: 0.42-7.02) without these associations being statistically significant.
Drug selling on the part users was reported as 63.4%, and a less common practice was to get paid for injecting someone else (21.5%). The latter practice increases 2.27 times the probability of having HIV compared to not doing it (RPc=2.27, 95% CI: 0.52-9.84); said association was not statistically significant.
When asking about HIV knowledge before starting to inject drugs, 85% of the people referred having previous knowledge, with this information being obtained in education institutions 54% of the time. Among the reported knowledge about HIV, 66% said they knew that not sharing injection equipment could prevent infection 2.02 times when compared with sharing the equipment (RPc= 2.02, 95% CI: 0.49-8.32). In regard to living with HIV, 96.6% were concerned.
When talking about reported practices in the last six months, it was found that 38.8% have shared needles and syringes with up to three people, followed by more than three people with 23.2%, and only 13.8% reported not having shared with anyone. Likewise, when comparing the fact of sharing with more than three people, we found that they were 5.07 times more likely to get the infection compared to those who do not share with anyone (RPc=5.07, 95% CI: 1.19-21.55). For the question of whether when they shared syringes they did it with a close friend, if the answer was always, they were 10.69 times more likely to get HIV compared to almost always (RPc=10.69, 95% CI: 2.26-50.61). Said associations were statistically significant (p<0.05) (table 2).
Table2 Factors>associated to the presence of HIV infection in people who inject drugs in the city of Medellín. December 2017 - January 2018.
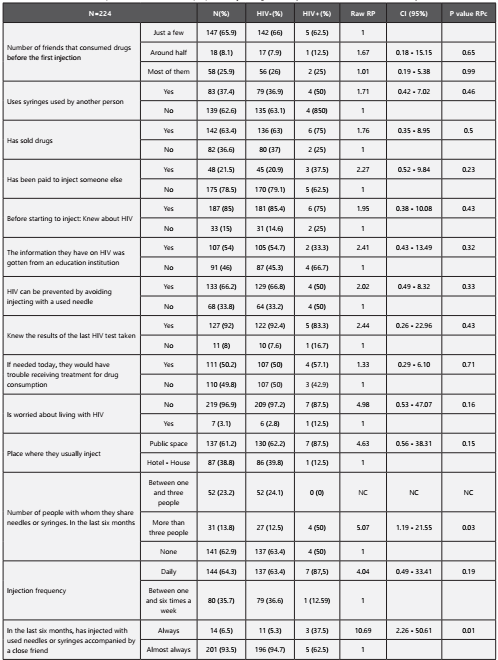
*NC: Not calculated
For the multivariate analysis, we included the variables: number of people with which they shared needles or syringes (in the last six months), and whether they have injected with used syringes accompanied by a close friend by statistic criterion of p<0.05. Additionally, we added the variables: has been paid to inject someone else, is worried about living with HIV, place where they usually inject, and injection frequency, by Hosmer and Lemeshow criterion. When adjusting the RP through the logistic regression method, two variables retained the condition of increasing the probability of HIV: place where they usually inject (public space), and has injected with used needles and syringes accompanied by a close friend. Nevertheless, none of them was statistically significant (table 3).
Discussion
In this research, we found that the majority of the participants were men with a 6:1 ratio, data which is similar to what was reported in the study by Berbesi-Fernández, et al, with a ratio of eight men per each woman5. In the heroin report in Colombia that consolidates the information of all studies carried out until that moment, which was published in 2015, they found a ratio of five men per each woman6.
Regarding socioeconomical stratum, 75% belonged to les privileged strata (low and very low), similar to what was reported by Mateu-Gelabert, et al. in a study done in Pereira and Medellín, where the percentage was 77%15. In regard to marital status, eight out of every 10 PWID in this study stated they were single. This result matches the data of the study by Berbesi-Fernández, et al., which reported a similar figure 3.
As to health registration, in this study we found that 65.6% of the population was registered in the subsidized regime. This result is comparable to the CES series between 2011 and 2014, which was reported in the heroin analysis in Colombia, showing 59.4% of the population in Medellín. Additionally, these two studies agree on the percentage of registered users in the contributory regime, which were 15.6% and 15.3%, respectively6.
Concerning the prevalence of HIV in PWID in the city of Medellín (3.6%), we found that is it higher compared to the report by Berbesí D, et al in 2010, which was only 2% 2, and subsequent studies (2014) showed an increase of up to 6.3%. These data confirm that the prevalence of the infection is low compared to other regions, as reported by United Nations Office on Drugs and Crime (ONODC) in 2016: Africa 11.2%, Asia 12%, and Europe up to 19.1%.
Regarding the consumption related to the risk of infection with HIV, we observed there was a higher prevalence in people who injected daily, as evidence in other studies, such as the report by Ospina-Escobar and Jarlais D14,15.
In this study we showed that there is a significant association between HIV infection and intravenous drug injection with used needles or syringes, which is similar to the results in various studies carried out by the National Health Ministry in Ukraine10,16.
Furthermore, we found that not only sharing equipment was a predisposing factor, but also sharing needles with multiple PWID; for this study, there was a higher chance of presenting with HIV infection when the number was more than three people. In the article by Des Jarlais D, et al., they found a comparable situation in which among the variables that influenced the emergence of new waves of infection by HIV, they included having broad injection networks as a predisposing factor. This is also supported by the report by Phukan S15,17.
This research showed that sharing and reusing injection equipment are associated to the presence of HIV infection. Keeping in mind that strategies to minimize the risk have been described around the world, it is necessary to systematically and regularly adopt those strategies in countries like Colombia, especially in cities like Medellín, since this will reduce the behaviors associated to the presence of the infection. It is essential to implement programs to reduce the harm, including addiction control, promotion of appropriate injection, and peer education to significantly decrease infection rates12.
Conclusion
Injecting drug use has been considered a problem of global public health interest, not only due to its physical and mental consequences, but also because this practice entails a risk of infections like HIV, viral hepatitis, among others. This is a worldwide concern given the fact that this practice is increasingly common among consumers, generating a global warning and the need to develop strategies to protect this population. Among these strategies, there are programs that aim at establishing safe injection methods and practices to protect the health of the consumers. It is now clear that they are not limited to stopping consumption (which is the most difficult objective to attain), but they go as far as recognizing addiction as a health issue. As expected, the inclusion of these programs has not occurred in the same way in all countries; in Colombia, some approximations have been carried out, but they have not been implemented systematically yet.
Punitive approaches aimed at the consumers of psychoactive substances have been known to increase unsafe practices that could mean a rise in the prevalence of HIV infection. On the other hand, if a public health approach is used, strategies that are effective and move toward reducing the damage associated with those practices could be used. As part of the intervention, educational and sterile injection material Access strategies may be put in place to mitigate the damage caused by consumption, as well as reducing costs for the health system in the medium and long-term.
In light of the low prevalence of HIV infection reported in this study, we consider it necessary and appropriate to develop and implement public policies whose objective is to créate prevention and education programs that will eventually lead to the reduction of HIV infection in people who inject drugs, after being refined and adjusted to local needs.
Limitations
Sampling based on the interviewee is considered a type of non-randomized selection that must comply with a series of assumptions to be considered a dependent sample of the social network. This study was not able to include PWID from high socioeconomical strata due to their lack of interest in receiving any kind of incentive for participating in the research.















