Introduction
The coronavirus disease 2019 (COVID-19) was originally identified in the city of Wuhan, China, in December 2019. Current evidence indicates that the COVID-19-causing virus is transmitted person-to-person through direct contact and droplets. People with the highest risk of infection are those who are in contact with and/or take care of COVID-19 patients, which inevitably places healthcare workers at a high infection risk1.
COVID-19 disease, which shows severe clinical manifestations such as severe acute respiratory syndrome by coronavirus 2 (Sars-CoV-2), was declared a global pandemic by the World Health Organization (WHO) in March 20202.
The Center for Disease Control (CDC) reported 907,003 COVID-19 cases of healthcare workers in the United States in 2020, of which 2,302 died3.
The COVID-19 pandemic has also had a disproportionate effect on female health workers. Women represent 70% of the global health and social care workforce, putting them at a higher risk of infection and a range of physical and mental health problems associated with their role as health professionals and caregivers in the context of a pandemic4. Healthcare workers face a high risk of infection due to close contact with potentially infectious patients and/or co-workers.
During the first wave of the pandemic and due to the little epidemiological evidence available, preventive measures were not adequately applied. The absence of an adequate clinical environment and the lack of experience in the clinical management of this new disease and personal protective equipment could have increased the risk of infection among health workers5.
Due to its high infection and transmissibility capabilities, it is essential to determine the characteristics of Sars-CoV-2 that increase the risk of health workers to get infected during the exercise of their daily tasks. Therefore, this study was aimed at estimating Sars-CoV-2 infection rate in employees of a hospital of medium and high complexity level according to their job responsibilities.
Materials and methods
An observational prospective cohort study was carried out with employees of the Tomas Uribe Uribe Departamental Hospital (TUUDH), which is classified as a medium and high complexity institution from Tuluá, Valle del Cauca (Colombia), using as a starting point the date when the first employee was diagnosed with COVID-19.
From this date on, the authorities decided to carry out diagnostic tests on hospital workers for COVID-19 infection. Thus, 1001 employees were tested using antigen and PCR based techniques during the study period of June 13, 2020 to October 15, 2021.
Various activities were conducted in order to identify new cases, including health questionnaires published by the Ministry of Health, a hotline, epidemiological investigations in order to identify clusters of cases or groups of workers exposed to a diagnosed case, and contact tracing of positive people.
Laboratory tests were available for all hospital personnel regardless of their vaccination status, following the guidelines of the Ministry of Health6.
Data collection and quiality control plan
The data was extracted from the information registered daily in the database of the epidemiology group of the hospital. Also, the data was collected about the variables of interest for the study: (i) age at the moment of the analysis (continuous and categorical). Thus, three categories were established: young people between 20 and 38 years old; young adults between 39 and 56 years old; and older adults aged 57 and over; (ii) gender; (iii) type of job, including patient care (responsible for direct care of patients, such as doctors, nurses, nursing assistants, physiotherapists, etc.), administrative (office activities, such as area managers, secretaries, lawyers, engineers, messengers, etc.), and operational (support activities like construction workers, drivers, security guards, etc.); (iii) study starting date; and (iv) date of diagnosis of Sars-CoV-2 virus infection.
The data processing went through three sequential phases: (i) database review and cleanup in order to resolve inconsistencies and missing data; (ii) database digitization using 2010 Microsoft ExcelTM, with double entry for quality control purposes; and (iii) record coding and export of statistical packages for the application of statistical procedures.
Statistical analysis
The frequency of variables and detection of atypical or extreme values were analyzed in order to analyze distribution and magnitude of the infection among workers. Each variable was analyzed according to its measurement scale, as follows. Frequency tables were used for qualitative variables (nominal and/or ordinal) in order to assess the frequency and distribution of the event of interest in the study population, and their proportions were estimated.
While central tendency, asymmetry, and dispersion measures, as well as interquartile range were estimated for quantitative variables measured as intervals or ratios, as appropriate. The data was examined through histograms, boxes and whiskers, and stems and leaves, which facilitated the identification of extreme and missing values. Results not shown in this manuscript.
For contrast analysis, the Chi-square and Student’s T tests were used for categorical and quantitative variables, respectively. The statistical decision was made based on an α=0.005 significance level. The infection positivity rate and cumulative incidences were estimated for the variables of interest.
Finally, the Kaplan-Meier statistic was used to compare the estimated infection rate between the categories of the variables of interest, using the log-Rank test. An α=0.05 was used to determine statistical significance6,7,8,9.
All cases that could not be established whether they had Sars-CoV-2 infection during the study period were eliminated from the analysis.
Statistical procedures were conducted using the SPSS® version 26 and SASTM version 9.0 statistical packages.
Ethical considerations
The Committee for Ethical and Scientific Evaluation of Research in Human Beings (or with a sample of human beings) of the Tomas Uribe Uribe Departmental Hospital de Tulua - State Social Enterprise approved the study protocol as stated in the minutes No. 01 of March 16, 2022. Informed consent was not required as the data was anonymous and no personal identifiers were collected.
Results
The pyramid of employees and population of workers show the total and within it the total of infected workers, both men and women. Among women, the groups with the greatest contribution to the infection burden (cumulative incidence) were the 24-29, 19-23, and 29-34 age groups, with percentages of 12.7%, 13.1%, and 9.8%, respectively. Whereas in men, the greatest percentages were observed in the 24-29 (5.6%), 29-34 (4.3%), and 35-39 (4.3%) age groups.
This finding indicates that infection is more frequent among younger groups. The variable of the abscissa axis represents percentage of people positive for the infection and totals in each group, according to gender (Figure 1).

Figure 1 Total employees and total employees infected with Sars-CoV-2. TUUDH. March 2020 - October 2021.
636 (63.7%) and 364 (32.4%) out of the 1001 employees who worked during the study period were women and men, respectively. Among those belonging to the patient care group, the average age and standard deviation for female were 36.6 and 10.5 whereas for men were 39.3 and 12.2, respectively, and this difference was statistically significant (t=2.3; gl=593; p=0.006). In reference to the administrative group, the average age and standard deviation were 44.1 and 12.3 for men and 39.8 and 10.5 for women, respectively.
This difference was also significant (t=2.3; gl=161; p=0.022). Finally, in the operational group, the average age and standard deviation were 46.1 and 12.0 for male and 43.5 and 12.4 for female employees, respectively. However, this difference was not statistically significant (t=0.85; gl=83; p=0.4).
When age was categorized, women represented 50.5%, 34.5%, and 15.5% of the youth, young adult and older groups, respectively. It is important to highlight that 84.5% of women are under 56 years old. In contrast, men accounted for 44.1%, 38.3%, and 17.6% of the same respective groups, and 82.4% of them are under 56 years old. These figures indicate that the hospital workers are mostly younger.
The difference in terms of infection rate between the three age groups was statistically significant (Log Rank=13.2; gl=2; p=0.001). The median infection rate was 16.0 weeks for young adults, 14.0 for older adults, and 15 months for the younger group. The assessment of the infection rate between young and young adults did not show a statistically significant difference (Log Rank=0.24; gl=1; p=0.63).
When comparing the young and older adult groups, a statistically significant difference was observed (Log Rank=18.6; gl=1; p=<0.0001), and a similar result was obtained when comparing young adult and older adult groups (Log Rank=10.6; gl=1; p=<0.0011) (Figure 2).
In terms of Sars-CoV-2 infection based on gender, the positivity and cumulative incidence rate in women were 27.0% (172/637, IC95% 23.6-30.5) and 21.2% % (77/311, IC95% 20.0-25.4), respectively, while in men the difference was significant (Chi2=4; gl=1p; p=0.04). The total cumulative incidence was 24.9% (249/1001 IC95% 22.2-27.6). The rate of infection occurrence was not statistically significant (Log Rank = 0.02; gl=1; p=0.89). The median infection rate was equal in both genders (16 weeks) (Figure 3).
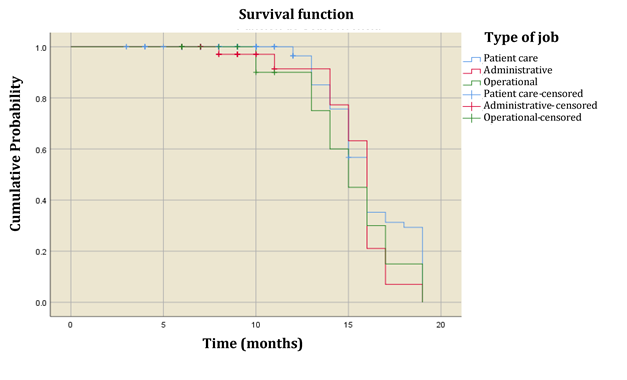
As described before, employees were classified as patient care, administrative and operational based on their job responsibilities. Women represented 75.8% (416/549), 19.7% (108/549), and 4.6% (25/549) of the patient care, administrative, and operational groups, respectively. On the other hand, male workers accounted for 60.9% (179/294), 18.7% (55/294), and 20.4% (60/294) of the patient care, administrative, and operational groups, respectively. Sars-CoV-2 infection in the patient care group was 27.6% (180/652), in the administrative group was 24.1% (46/191), and in the operational group was 17.0% (18/106).
The difference in infection between these three groups was statistically significant (Chi2=53.8; gl=2; p=0.000). Although the Sars-CoV-2 infection rate did not show a statistically significant difference, the median infection for patient care and administrative workers was 9 weeks, whereas this figure for the operational group was 10 weeks (Log Rank=0.16; gl=2; p=0.92)(Figure 4).
Discussion
In the patient care group, the average age was 36.6 years for women and 39.3 years for men and the difference was statistically significant (t=2.3; gl=593; p=0.006). The administrative group showed average ages of 39.8 and 44.1 years for female and male employees, respectively, and the difference was statistically significant (t=2.3; gl=161; p=0.022). Finally, in the operational group the average was 43.5 and 46.1 years for women and men, respectively, however, this difference was not statistically significant (t=0.85; gl=83; p=0.4). This finding indicates that the population of employees is mostly female and young, with women being younger than men on average.
When age was re-coded into three equal groups, young (20 to 38 years), young adult (39 to 56 years), and adults (57 and over), the Sars-CoV-2 infection rate between these three age groups was statistically significant (Log Rank=13.2; gl=2; p=0.001) and the median infection rate was 16.0 months for young adults, 14.0 for older adults and 15 weeks for the young. These results indicate that the three groups show differences in terms of infection, with older adults being the most susceptible.
Statistically significant differences in terms of infection rate between the young and elderly group were observed, being higher in the latter group (Log Rang=16.6; gl=2; p≤0.0001). The same situation is observed when the young adult and elderly groups are compared, indicating that older adults are more susceptible to Sars-CoV-2 virus infection (Log Rang=10.6; gl=2; p≤0.0011). In fact, the median infection rate is 16.2 for the young, 16.8 for the younger adult, and 14.3 for the older adult groups.
The overall cumulative infection rate based on gender was 24.9% (24.9/1001, 95%CI 22.2-27.6). Positivity in women was 27.0% (172/364 95%CI 23.6-30.5), whereas in men was 21.2% (77/364 95%CI 20.0-25.4) and this difference was statistically significant (Chi2=4.2; gl=1; p=0.04). However, there was no statistically significant difference when infection rate was compared between female and male study participants (Log Rank=0.02; gl=1; p=0.89). This finding suggests that both men and women were infected, on average, at the same rate and the fact that the median infection rate was 16.0 weeks for both genders confirm what has been said, indicating that 50% of both working men and women had already been infected at that time.
Sars-CoV-2 infection in the patient care group was 27.6% (180/652), in the administrative group was 24.1% (46/191), and in the operational group was 17.0% (18/106). The difference between these groups was statistically significant (Chi2=53.8; gl=2; p≤0.0001). Despite this significant difference, the Sars-CoV-2 infection rate did now show a statistically significant difference. The median infection was 10.0 for the three job groups (Log Rank=4; gl=2; p=0.12).
A study carried out on hospital workers reported a cumulative incidence of 11.2% (65/578, 95%CI 8.8-14.1)12, which lower to that observed in this study which was 24.9% (249/1001; 95%CI 23.5-26.3). The cumulative incidence obtained in our study is higher and reaches one in four active workers.
Another study carried out in the largest hospital in New York City reported a prevalence of 13.7% of antibodies against Sars-CoV-2, which is similar to the prevalence (14%) found in a randomized study also done in New York City. However these results are higher than the prevalence reported in a study conducted in the city of Los Angeles (4.1%). A hospital in Belgium reported a 6.4% prevalence. A study carried out in Sweden on 2,149 hospital workers reported a 190% prevalence. All these figures are lower than the cumulative incidence reported in this study13,14,15,16,17.
A study conducted in three states of the United States reported that 69.6% of 24,749 hospital employees were younger than 50 years and 78.2% were women18. This result is similar to our data showing that 63.6% of the study participants were women and 84.5% were younger than 56 years.
In Brazil, a study on 1,525 health workers reported a distribution of 525 medical doctors, 471 registered nurses, 263 nursing assistants, and 264 physiotherapists19. Although the authors found that women predominated in all categories (81.1%; 95% CI: 77.8% to 84.1%), their percentages are much higher than the ones observed in this study (63.6%; 95% CI: 59.9-67.3).
Previous evidence indicates that age and gender are important factors in the occurrence of Sars-CoV-2 virus infection. Nevertheless, this situation may be a consequence of the composition of the health labor force, particularly in developing countries where the majority of workers tend to be female.
It is noteworthy that we have not found any difference in terms of the type of work performed within our categories of patient care, administrative or operational, given that patient healthcare workers have close and lasting contact with patients. A possible explanation for this finding could be that administrative employees are in contact with patients’ relatives and some of them either may be asymptomatic or are incubating the infection, but they can also transmit the virus.
Consequently, these findings highlight the occupational risk of Sars-CoV-2 infection among healthcare workers. Thus, it is important to maintain safety measures to reduce the risk of infection.
Limitations
The fact that this study did not assess variables such as length of time in the current job made it difficult to accomplish a more detailed analysis of the effect of time on the labor situation. Likewise, the tests carried out during the study changed from almost exclusively serological at the beginning to PCR-based techniques at the end. This change meant that not all workers were diagnosed with the same test and this could introduce a certain percentage of false negative and positive results.