Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Aquichan
Print version ISSN 1657-5997
Aquichan vol.7 no.1 Bogotá Jan./June 2007
How Many Nurses are Enough? A pilot Study Measuring Nursing
Care Hours per Patient Day and Patient Outcomes
¿Cuantas enfermeras son suficientes? Estudio piloto diseñado para evaluar la relación horas
de cuidado a cargo de enfermeras y mejoría de los pacientes, por día
Quantas enfermeiras bastam? Um estudio piloto medindo horas de cuidado
diárias por paciente e resultados de paciente
Peggy Tallier, EdD, RN*
Department of Nursing Graduate Studies Lehman College , City University of New York , USA . ptcvigilancehealthcare.com
ABSTRACT
The In this article, the author presents research and findings of correlations between patient outcomes and staffing mix, in particular, the proportion of Registered Nurses and its impact on quality of care. In examining the relationships among nursing quality indicators of care, the investigator focused on the mix of Registered Nurses, Licensed Practical Nurses, and unlicensed staff; the maintenance of skin integrity; and the link between nosocomial urinary tract infections and patient satisfaction for patient outcomes. The results indicate that adequate nurse staffing and appropriate skill mix is an important factor to consider when making critical staffing decisions. The study also demonstrated statistically significant relationships among the proportions of Registered Nurses and nosocomial urinary tract infections and patient satisfaction
KEYWORDS
Staffing mix, quality of care, impact, care outcomes
RESUMEN
En este artículo la autora presenta la investigación y los hallazgos de la correlación mejoría de los pacientes/diversidad de personal, en particular la proporción de enfermeras registradas y su impacto en la calidad del cuidado. Al examinar las relaciones entre los indicadores de calidad del cuidado prestado por enfermeras, la investigadora se concentró en la mezcla de enfermeras profesionales registradas, y personal no profesional, en el mantenimiento de la piel, y en la relación entre infecciones hospitalarias del tracto urinario y la satisfacción de los pacientes por su mejoría. Los resultados señalan que el adecuado número de personal de enfermería y la apropiada mezcla de habilidades son factores que se deben tener en cuenta al tomar decisiones importantes acerca del tipo de personal. El estudio también demostró relaciones estadísticamente significativas entre la proporción de enfermeras registradas, las infecciones hospitalarias del tracto urinario y la mejoría de los pacientes
PALABRA CLAVE
Diversidad de personal, calidad del cuidado, impacto, resultados del cuidado.
RESUMO
Este artigo apresenta a pesquisa e as co-relações entre resultados do paciente e composição do pessoal, em especial a proporção de enfermeiras registradas e seu efeito na qualidade do cuidado. Ao examinar as relações entre indicadores da qualidade do cuidado, o pesquisador deu importância ao pessoal de enfermeiras registradas, enfermeiras práticas com licencia e pessoal no licenciado; manutenção da integridade da pele e a relação entre infecções nosocómicas do trato urinário e satisfação do paciente por seus resultados. Os resultados revelam que, na tomada de decisóescríticas sobre pessoal, selecionar o pessoal adequado de enfermeiras com a mistura apropriada de habilidades é um fator importante. O estudo amostra, ademais, relações estatisticamente significativas entre proporção de enfermeiras registradas e infecçõ es nosocómicas do trato urinário, e satisfação do paciente
PALAVRAS-CHAVES
Composição dopessoal, qualidade do cuidado, efeito, resultados do cuidado.
Rapind apid and seismic changes in the healthcare industry, which are not just unique to the United States , have put patient safety and the quality of care at risk in hospitals today. The nursing shortage, frequent restructuring, downsizing, and cost containment efforts often occur without anticipating or planning for the adverse impacts these changes have on patient careo The ever-growing demand to economize in the provision of care continues at an unprecedented rate and remains a constant pressure on healthcare administrators
Among the many significant pressures hospitals must address are the economic determinants that influence staffing patterns and staffing regulations. In 1997, Buerhaus cited significant factors that contribute to the overall fragmentation in standardized staffing regulations, factors that continue to affect an already stressed system today. As he noted, when compensation rises over time, hospitals are forced to hire fewer staff. Out-of-control labor market shortages in nursing continue to vex all aspects of healthcare delivery. Hospitals are challenged to juggle the relationships among capital and labor and their associated expenses, while fashioning a delicate balance between cost saving and compromising patient ea re. In the end, hospitals must meet the challenge of determining what combination of nurses and other healthcare personnel provide optimal output.
In the middle of this crisis sits the profession of nursing. Nursing leaders are continual/y being called upon to devise creative staffing methods and to find ways" to do more with less.1I Nurse executives must be able to quantify the number of nurses needed to assure safe, qua lit y care and substantiate how nursing interventions are linked to patient outcomes.
To develop effective partnerships with hospitals and to meet these challenges, nursing must shift away from staffing patterns based on nonfunctional, outdated industrial models that focus on work sampling and time-in-motion studies to a professional model. Outmoded nurse-to-patient ratios can no longer be used as a baseline standard for minimum safe staffing in order to adequately evaluate and implement a professional staffing model. Nursing interventions and their impact on patient outcomes must be measured using nursing-sensitive quality indicators and must be based on the intensity and complexity of care needed for each patient.
The turmoil that has accompanied the recent changes in healthcare provides an opportune time for the profession of nursing to evaluate current practices and to explore a number of essential questions regarding staffing ratios. It is this investigator's belief, however, that before a paradigm shift is possible, executives and nurses must have a better understanding of how nurse ratios affect patient outcomes. To that end, this study seeks to provide the profession of nursing with data that incorporate structure, process, and outcome indicators strongly linked to nursing care, as well as information that may assist in defining the relationships among staffing and patient outcomes. As cost-containment measures continue to bedevil the system, this work may provide valuable support to nurse executives in helping to manage fiscal responsibilities that affect the quality of care. And, as the prevailing urgency continues to force the healthcare industry to economize in the provision of care, it is imperative that nursing contributes in significant ways to positive patient outcomes
Contex for Study: Cost Savings anf Patient Outcomes
Sinces nurses are the single-Iargest labor cost for hospitals, representing one-fourth of the hospital's workforce, the profession of nursing is increasingly vulnerable and at risk for budget cuts in today's market-driven setting. Indeed, hospitals are looking at the cost of Registered Nurses and using this as the primary cutback in an effort to remain competitive. These pressures ha ve led to an increased workload on professional nurses and have significantly lowered the number of licensed personnel in many hospital settings.
How are these cost-saving cutbacks affecting patient outcomes? Despite widespread changes in the delivery of nursing care, the effects on patient outcomes have not been studied sufficiently". As media coverage increases and dissatisfaction and concern by the public grows, the federal government and a number of states are responding to the cutbacks with new laws mandating minimum nurse staffing levels, measures that provide no clear answers. Will solely increasing the number of licensed personnel or mandating minimum staffing levels solve these complex issues? The question that still remains to be addressed is how many nurses are enough.
Decisions about the adequacy and appropriateness of nurse staffing have long been based on functionally outdated industrial models that focus on work sampling and time-and-motion studies conducted in semi-simulated settings. Even today, the common method of staffing nursing units or identifying the staffing mix in hospitals is by identifying budgeted Nursing Care Hours per Patient Day. A traditional measure of nursing productivity, nursing hours per patient day has never been satisfactory because 'patient day' as a measure of nursing output takes neither patient acuity nor quality of nursing care into accou nt". .
Thus costly and critical budgetary decisions are dependent on a staffing method that does not account for important factors such as individual and aggregate patient needs or unit functions. Although suggestions to use acuity levels as nursing output measures continue to be presented, patient acuity systems tend to measure what patients need rather than what care is actually delivered.
Nursing services are a series of multifunctional assessments, actions, and interventions that are clearly related to patient outcomes. Yet, as a profession, nursing remains unable to support these efforts with accurate standardized data. The challenge, then, is to successfully demonstrate these outcomes in terms of language and definitions that foster and support critical decision-making and become nationally accepted indicators. Unless nursing-specific contributions are identified, nurses' role in providing healthcare will remain invisible and ultimately unsupported".
Nursing-Sensitive Quality Indicators of Patient Care
Units that rely solely on Nursing Care Hours per Patient Day to determine appropriate staffing levels are not utilizing an effective or practical way to make critical staffing decisions. Over the last decade, researchers have begun to investigate how to assess the outcomes of nurses.
Jennings-Mowinski, Staggers, and Brosch conducted an intensive review of the literature beginning in 1974 in the areas of medicine, nursing, and health services research to identify outcome indicators. The researchers suggested that having an understanding of the complexities in selecting indicators maximized the potential for success in outcome measurement.
Further studies reveal the link between increased nursing care and better patient outcomes in hospitals, and there is strong reinforcing evidence that relationships between nurse staffing and adverse patient outcomes exist. Although the studies vary, there is sufficient information to suggest that higher Registered Nurse staffing ratios are related to a number of positive patient outcomes. However, data supporting specific nurse-to-patient ratios are not yet available.
To remedy the shortcoming in research data, nursing-sensitive indicators are now becoming the focus of study to determine staffing patterns and patient outcomes. As defined by Lichtig, Knauf, and Millholland, nurse-sensitive indicators are patient outcome measures that may be influenced by nursing interventions. Lichtig et al. examined publicly available data on a state-to-state level and concluded that adverse patient outcomes, defined by nursing-sensitive quality indicators, are significantly related to lower Registered Nurse proportions in hospitals. In 1999, Blegan et al. reported similar results in their study. Still, other investigations have found significant negative relationships between nurse staffing and adverse patient outcomes: Higher Registered Nurse staffing was associated with a 3-12% reduction in specific . adverse outcomes and higher staffing at all levels was associated with a 2-25% reduction in adverse outcomes.
For a decade, the American Nurses Association and the American Organization of Nurse Executives have recommended the use of nursing-sensitive quality indicators, such as nosocomial infection rates, patient falls, medication errors and nurse satisfaction studies, as starting points for data repositories. In March 1994, the American Nurses Association Board of Directors initiated a multiphase study (Nursing Report Card for Acute Care Settings) to investigate the impact of restructuring on the safety and quality of patient care, as well as its effects on nursing. The result, Nursing Quality Indicators: Definitions and Implications and the Guide for Implementation, was published in June 1996, along with a national database of nursing-sensitive qua lit y indicators that included: 1) the mix of registered nurses, licensed practical nurses, and unlicensed staff caring for patients in acute-care settings; 2) total nursing care hours provided per patient day; 3) pressure ulcers; 4) patient falls; 5) patient satisfaction with pain management; 6) patient satisfaction with educational information; 7) patient satisfaction with overall care; 8) patient satisfaction with nursing care; 9) the nosocomial infection rate; and 10) nurse staff satisfaction.
In 1998, the American Nurses Association provided funding to develop a national database to store the nursing sensitive quality indicators. The database is jointly managed at the Midwest Research Institute in Kansas City , Missouri , and at the University of Kansas School of Nursing. The goals of establishing the database are to promote and facilitate the standardization of information submitted by hospital s across the United States on nursing quality and patient outcomes. Important features of the database include nursing-sensitive data that is collected and reported at the unit level and stratified by type of unit and size of hospital; confidential benchmarking reports are provided to the participating hospitals. Notably, on July 1, 2002, the Joint Commission on Accreditation of Health Organizations began to survey hospitals for compliance with the organization's new effectiveness standards. Utilization of nursing-sensitive quality indicators presents an effective strategy for providing the clinical data the Joint Commission now requires to meet these standards.
Quality is a difficult term to define in relation to healthcare. However, as Donabedian concluded, this definition is necessary to provide a framework for additional methods and measurements of assessment He postulated that the basic elements of a definition of qua lit y begin with the simplest module of patient care; that is, the management of a patient by a primary practitioner during a definable episode of illness. The degree of quality is the extent to which the care provided is expected to achieve the most favorable balance of risks and benefits.
Donabedian posited that quality can be measured through what he termed structure, process, and outcomes. Similarly, Irvine , Sidani, and McGillis Hall proposed a theoretical framework using the Nursing Role Effectiveness Model, which presented patient care as a multidisciplinary function in which many providers are interacting and delivering care for the purpose of achieving desired outcomes. This model demonstrated nurses' roles in healthcare and related these roles to specific patient and cost outcomes.
For Irvine et al., the structure component consists of nurse, patient, and organizational variables that influence the processes and outcomes of care, while to Donabedian, structure is "the relatively stable characteristics of the providers of care, of the tools and resources they have at their disposal, and of the physical and organizational settings in which they work. .. that is, "the human, physical, and financial resources that are needed to provide medical ea re". The structure indicators employed in this study were Nursing Skill Mix; that is, the ratio expressed in Full-Time Equivalents (FTEs) of Registered Nurses with direct patient-care responsibilities to Licensed Practical Nurses and unlicensed personnel on acute-care units. Total Nursing Care Hoúrs Provided per Patient Day refers to the total productive hours worked by nursing staff with direct patient-care responsibilities working on acute-care units per patient day.
The process component, according to Irvine et al, refers to nursing's independent, dependent, and interdependent roles, and how they influence outcomes of care, while for Donabedian process meant "a set of activities that goes on within and between practitioners and patients". Irvine et al. suggested that it is important to identify and investigate nursing-sensitive quality indicators that are guided by a conceptual framework that can establish relationships between nursing care and patient outcomes. "Outcomes are affected not only by the care provided, but also by the factors related to the interpersonal aspects of ea re, and to the setting in which care is provided". The process indicator reviewed in this study was Maintenance of Ski n Integrity, referring to the rate per 1,000 patient days at which patients develop pressure ulcers (Stage 10r greater) during the course of their hospital stay, but 72 hours or more following admission. For this study, pressure ulcers are defined as a localized area of tissue disturbance that develops when soft tissue is compressed between a bony prominence and external surface for a prolonged period of time. Pressure ulcers are staged from I to IV to classify the degree of tissue damage observed.
The outcome component defined by Irvine et al. applies to nursing-sensitive patient outcomes such as general patient state, behavior, or perception resulting from nursing interventions, clinical symptoms, and patient knowledge, while Donabedian described outcome simply as "a change in a patient's current and future health status that can be attributed to antecedent health care". Outcome indicators in this investigation included Nosocomial Infection Rate and Patient Satisfaction with Nursing Careo Nosocomial Infection Rate refers to the rate per 1,000 patient acute days at which patients admitted to acute-care settings develop urinary tract infections (including symptomatic urinary tract infection, asymptomatic bacteriauria, and other infections of the urinary tract, Le., kidney, ureter, urethra, or tissues surrounding the retroperitoneal or perinephric spaces or other infections of the urinary tract as defined by the Centers for Disease Control) following the first 72 hours of the hospital stay and for which there is no evidence to suggest the infection was present or incubating at admission.
Patient satisfaction is widely defined and recognized for this investigation as a patient's opinion of the care received during the hospital stay as determined by scaled responses to a uniform series of questions designed to elicit patient views regarding various aspects of care.
Methods
The methods selected to implement the study included four separate instruments. The overall design used to collect patient data was retrospective analysis and patient medical record review. The sample of convenience consisted of all adult male and female patients admitted to the hospital between October 1, 2000, and March 31, 2001. AII nurses participating in the study worked on the units during the period from October 1, 2000 through March 31, 2001
Population and Sample
The population for this investigation consisted of adult female and male patients age 18 or older admitted to the hospital in seven separate nursing units, five of which were general Medical-Surgical, one was the Intensive Care Unit, and one was a designated Geriatric Unit. These units were chosen as the study sites because all of the patients admitted were potential candidates for acquiring pressure ulcers and urinary tract infections. AII the patients in the study had a length of stay three days or greater, and all the patients diagnosed with nosocomial urinary tract infections or pressure ulcers during that time period were investigated
Instruments
The four instruments used to collect data were the Department of Nursing Daily Nursing Care Hours Sheets, the patient's medical record, hospital microbiology reports, and the Patient Satisfaction Survey.
The nursing administrative reports consisted of the Department of Nursing Daily Nursing Care Hour Sheets, with verification provided by the Department of Nursing Daily Nursing Staffing Sheets if any discrepancy was encountered; the Staffing Sheets were not used as a separate instrument to collect data. The Daily Nursing Care Hour Sheets illustrated hours worked per shift, unit census, and the exact number of staff working per shift and per unit by job classification. RNs, LPNs, and unlicensed nursing staff were separated by category and the total Nursing Care Hours per Patient Day were calculated using this report. The normal range of Nursing Care Hours per Patient Day was 4.0 to 12.0.
The Nursing Staffing Sheets were used only to validate the total Nursing Care Hours per Patient Day and to calculate the Registered Nurse ratio to other nursing staff, not as a separate data-collecting instrument. This report included specific information about the categories of staff working in each individual unit, unit census, and the hours worked for each individual staff member. This report was generated daily and was used as a day-to-day operational staffing instrument.
The patient's medical record, following guidelines established by the Agency for Health Care Policy and Research, provided data on nosocomial pressure sores. The State Department of Health and the Joint Commission on Accreditation of Hospitals require all hospitals to collect, aggregate, and analyze al! suspected nosocomial infections, including pressure ulcers. The data collected met al! required definitions of pressure ulcers as designated by the Agency for Health Care Policy and Research Guidelines.
Hospital microbiology reports, under the guidelines established by the Centers for Disease Control and Prevention, were used to collect data on nosocomial urinary tract infections. The State Department of Health regulations and the Joint Commission on Accreditation of Hospitals require all hospitals to collect, aggregate, and analyze all suspected nosocomial infections, including urinary tract infections. Al! patients diagnosed with a nosocomial urinary tract infection during the period from October 1, 2000 through March 31, 2001, were investigated.
Patient satisfaction was measured through a Patient Satisfaction Survey designed in 1999 by Health Care Systems Data. The survey was distributed to al! patients admitted to the hospital between July 1, 2000 and May 31,2001, by an outside healthcare consulting firm subcontracted by the institution. The survey was sent to all patients admitted to the hospital during this time with instructions and postagepaid return envelopes, and the completed surveys were returned directly to the consulting firm.
Every patient was mailed a survey in both English and Spanish. A total of 201 surveys were returned to the consulting firm. The survey consisted of 32 questions, 21 of which related to patient care and were measured in the investigation. Although the instrument consisted of nine sections, only six sections that pertained to nursing care were used: quality of care, patient preferences, emotional support, education, physical care, and discharge. The questions required either yes/no answers or asked about levels of satisfaction rated from 4 down to O, with 4 representing the highest score. yes/no questions were scored 1 or O, respectively. The scores ranged from 27 to O. There was no informátion available to the investigator regarding the reliability or validity of the instrument; however, the researcher and three other nurse experts in this area measured for content validity on a 4-point scale from 1= not relevant to 4 = very relevant. Content validity was reported at r =.90
Data Collection
The Department of Nursing Daily Nursing Care Hour Sheets and the Nursing Daily Staffing Sheets were obtained from the nursing administrative offices in the subject hospital. The data were collected retrospectively from October 1, 2000 through March 31, 2001, and analyzed solely by the investigator. Data from the patients' medical records and hospital microbiology reports were collected retrospectively from the Infection Control Reports from the Department of Microbiology and were retrieved through the Infection Control Department. Permission to use the Patient Satisfaction Survey data was granted by the hospital's on-Site Administrator and the Chief Bursing Officer.
All the data in this investigation were collected during the same time period, conducted on an ongoing basis during the months of April 2002 through August 2002. AII participants were volunteers who were guaranteed complete anonymity and provided a written description of the research study, as well as information on participants' rights and informed consent. AII participants were informed that they had the right to withdraw at any time and that they had the right to omit any question if they so chose
Data Analysis and Results of the Study
To support the premise of a relationship between nurse staffing and patient outcomes, six major findings emerged in this investigation. Data were reviewed from the fourth quarter of the year 2000; that is, from October 1, 2000 through December 31, 2000, to the first quarter of the year 2001; that is, from January 1, 2001 through March 31, 2001:
- 1. Although Nursing Care Hours per Patient Day were within the national standards for the nursing units investigated in this study, the category and type of staff fluctuated between the fourth quarter of the year 2000 and the first quarter of the year 2001.
2. No statistically significant relationship was found between the number of nosocomial pressure ulcers and Nursing Care Hours per Patient Day.
3. No statistically significant relationship was found between the number of nosocomial urinary tract infections and Nursing Care Hours per Patient Day
4. A statistically significant relationship was found between the number of nosocomial urinary tract infections and Registered Nurses.
5. No statistically significant relationship was found between patient satisfaction and Nursing Care Hours per Patient Day
6. A statistically significant relationship was reported between patient satisfaction and the cohort of Registered Nurses and Licensed Practical Nurses.
The data collected in this investigation were analyzed in light of the structure, outcome, and process indicators outlined earlier as a means for determining the Quality of care based on nursing-sensitive indicators.
Findings Related to Structure: Nursing Skill Mix
The rations of the nursing staff analyzed in this study relating to structure indicators included Nursing Care Hours per Patient Day; the mix of Registered Nurses, Licensed Practical Nurses, and Unlicensed Staff; and the Ratio of Registered Nurses.
Currently, the Nursing Care Hours per Patient Day formula is the unit of analysis that determines staffing requirements in hospitals. It is a calculable formula that is used as a method of staffing and for budgeting nursing hours (American Nurses Association, 1999). Nursing Care Hours per Patient Day are calculated by multiplying the number of staff delivering direct nursing care by the hours worked during the shift and then dividing that number into the average daily census at a specific designated time. For the purposes of this study, the midnight census was chosen as the designated time. Nursing Care Hours per Patient Day were studied and the data from both Quarters under review were analyzed and compared.
In this study, during the fourth Quarter of the year 2000, the average number of Nursing Care Hours per Patient Day was 5.91. During the first Quarter of the year 2001, the average number of Nursing Care Hours per Patient Day was 5.67. Although the average number of Nursing Care Hours per Patient Day was higher during the fourth Quarter of the year 2000 than the first Quarter of the year 2001, the percentage of Registered Nurses delivering direct patient care was, in fact, 3% lower in the fourth Quarter of the year 2000 than in the first Quarter of the year 2001. This illustrates the inconsistency of solely using Nursing Care Hours per Patient Day as the sole method of staffing patient units (table 1).
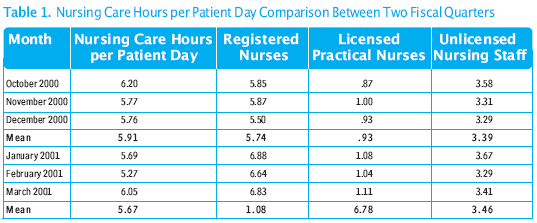
In this study, the categories of all nursing staff were analyzed and compared from the fourth Quarter of the year 2000 to the first Quarter of the year 2001, assessing for variations, fluctuations, and changes in nursing skill mix patterns. A comparison of the data from the two consecutive Quarters revealed fluctuations among all categories of staff, as well as the overall Nursing Care Hours per Patient Day (tables 2 and 3).


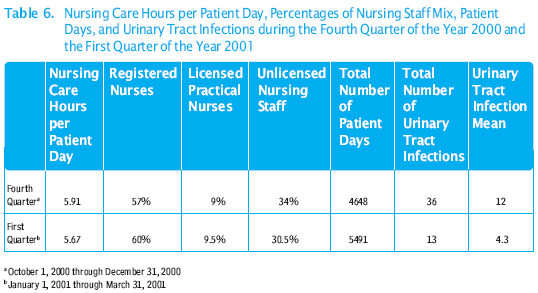
The fluctuations in staff types and numbers that were found were between the percentage of Registered Nurses in the fourth Quarter of the year 2000 (57%), with alto 9 nurse-to-patient ratio, and the percentage of Registered Nurses in the first Quarter of the year 2001 (60%), with alto 10 nurse-to-patient ratio. Differences between unlicensed nursing staff between the two Quarters also were reported. In the fourth Quarter of the year 2000, 34% unlicensed nursing staff was reported, and in the first Quarter of the year 2001, 30.5% unlicensed nursing staff was noted. Sovie has recommended at least a 70% Registered Nurse Staff for Medical-Surgical units and an 80% Registered Nurse staff for the Intensive Care Unit. The data highlighted in this study were below this recommendation in the Medical/Surgical areas. licensed Practical Nurse staffing remained constant during both Quarters and did not show a correlation with any of the dependent variables measured in the study, with the exception of patient satisfaction.
Findings Related to Process: Skin Integrity and Pressure Ulcers
MainMaintenance of ski n integrity and nosocomial pressure ulcers were defined as the process indicators in this study. This researcher hypothesized that there would be statistically significant relationships between a decrease in the proportion of Registered Nurses per Patient Day and nosocomial pressure ulcers. The study results did not support the hypothesis.
The total number of nosocomial pressure ulcers and the pressure ulcer rates were analyzed and compared between the two consecutive quarters. They were then further analyzed monthly, weekly and by incident, and the mea n was calculated. Eight nosocomial pressure ulcers with a mean of 2.67 were diagnosed during the fourth quarter of the year 2000. The Nursing Care Hours per Patient Day in the fourth quarter was 5.91, with a 57% Registered Nurse proportion and a 34% unlicensed nursing staff proportion. Sixteen pressure ulcers with a mean of 5.33 were diagnosed during the first quarter of the year 200l. Nursing Care Hours per Patient Day totaled 5.67, with a 60% Registered Nurse proportion and 30% unlicensed nursing staff during that quarter. Despite the higher proportion of Registered Nurses and pressure ulcer mea n during the first quarter, no statistically significant relationship was demonstrated. This may be related to the small sample size of pressure ulcer data collected in the study (table 4).

Although no statistically significant relationship was revealed, the findings show a tendency for pressure ulcer incidence to increase when the unlicensed staff is reduced. This is understandable, since the unlicensed staff's responsibilities include turning and positioning patients, which is one of the methods required to maintain intact ski n integrity. These tasks are not routinely the responsibility of the Registered Nurses in Medical/Surgical units.
During the time frame in which nosocomial pressure ulcers were studied, the sample size reported was small (n=24). Clinical evaluations are the responsibility of the Registered Nurse during routine patient care, including observations of pressure ulcers, which are then assessed and documented in the nursing record. Pressure ulcer predictor scales can be used to assess skin integrity and the potential risk of pressure ulcers. However, they were not used at this investigation site, possibly contributing to underreporting of the pressure ulcers in the patient's medical record.
No significant correlation was found between Nursing Care Hours per Patient Day and nosocomial pressure ulcers, using Pearson Product-Moment Correlation Coefficients (Table 5). However, the mean of nosocomial pressure ulcers did increase from 2.67 to 5.33 when there was a reduction in unlicensed staff from 34% to 30.5%. Future investigation into the relationship between Registered Nurses and pressure ulcers is suggested, because other studies have indicated lower incidence rates of pressure ulcers in units with a higher Registered Nurse proportion.

The findings here suggest that, in future studies, statistically significant results may be achieved if data are collected for twelve months rather than six months, providing there is a large pressure-ulcer sample size. Statistically significant results may also be achieved if a scale for predicting pressure-ulcer sore risk is used by the Registered Nurses for one year prior to the data being collected and analyzed
Findings Related to Outcomes: Nosocomial Urinary Tract Infections and Patients Tract Infections
This investigator's hypothesis presented no statistically significant relationship between the number of nosocomial urinary tract infections and Nursing Care Hours per Patient Day. However, the research did show statistically negative relationships between a decrease in the proportion of Registered Nurses per Patient Day and urinary tract infections, and the findings supported the hypothesis.
To gather data, the institution's Microbiology Infection Control Reports were audited during the time period under study. A total of 1,531 record s were reviewed and 312 urinary tract infections were diagnosed from these reports. Of the 312 urinary tract infections, it was determined that 49 were nosocomial urinary tract infections. Pearson ProductMoment Correlation Coefficients were employed to examine the relationship between the proportion of Registered Nurses and nosocomial urinary tract infections. The correlation between the number of Registered Nurses and nosocomial urinary tract infections was reported at p < .05. The findings suggested a relationship between the number of Registered Nurses delivering direct patient care and adverse patient outcomes such as nosocomial urinary tract infections. The findings also reported a negative relationship between Registered Nurses and urinary tract infections, implying that a skill mix that consists of 60% Registered Nurses may not be an adequate proportion of Registered Nurses to prevent nosocomial urinary tract infections (tables 6 and 7).
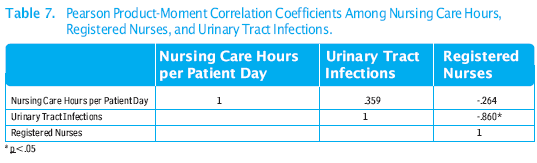
The findings here complement the work of Blegan et al., who completed a study that examined nurse staffing and patient outcomes. Their investigation reported that, as the proportion of Registered Nurses increased, rates of adverse outcomes decreased by up to 87.5%, concluding that the higher the percentage of Registered Nurses, the lower the number of poor patient outcomes, including such conditions as urinary tract infections and pressure ulcers.
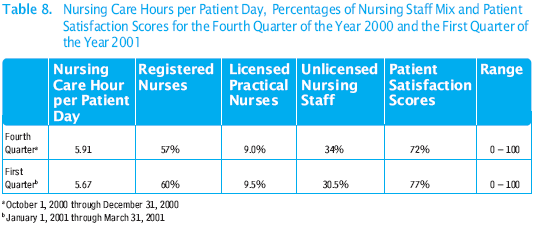
Patient Satisfaction
Patient satisfaction was the final outcome indicator included in this investigation. Although no statistically significant relationship was reported between patient satisfaction and Nursing Care Hours per Patient Day, a statistically significant relationship was found between patient satisfaction and Registered Nurses. The patient satisfaction scores in the fourth Quarter of the year 2000 totaled 72%, while the patient satisfaction scores in the first Quarter of the year 2001 were 77%. In the fourth Quarter of the year 2000, the number of Nursing Care Hours per Patient Day was 5.91, with the Registered Nurse proportion at 57%. In the first Quarter of the year 2001, Nursing Care Hours per Patient Day totaled 5.67 and the Registered Nurse proportion was 60%.
In the completed Patient Satisfaction Surveys, the respondents reported the most amount of dissatisfaction with the call-bell response time; education about the prevention of falls while in hospital; assistance with getting out of bed, eating and getting to the bathroom; and discharge planning. These components were scored at less than 48% of satisfaction for both Quarters. With the exception of discharge planning and education about the prevention of falls, Registered Nurses most often delegate these patient care responsibilities to the unlicensed nursing staff. This finding denotes an area for future research regarding the amount and types of staff needed to address the important but more basic needs of patients..
The patient responses relating to emotional support, patient education, and pain management were reported at 72% in the fourth Quarter with the Registered Nurse proportion at 57%, and a score of 77% in the fourth Quarter with the Registered Nurse proportion at 60%. The findings here suggested that the level of patient satisfaction is lower when there are fewer Registered Nurses available to meet higher-level needs of patients (table 8).
Implications of Findings and Recommendations for Research
In a 1996 report report titled "Nursing Staff in Hospitals and Nursing Homes: Is It Adequate?," the Institute of Medicine highlighted the need for ongoing data collection and research into staffing and other issues that affect patient safety and the Quality nursing care. Most recently, the Institute of Medicine released "Patient Safety: Achieving a New Standard for Care," a report that describes a detailed plan to facilitate the development of data standards applicable to the collection, coding, and classification of patient safety information. This report by the Institute of Medicine addresses key areas related to the establishment of a national health information infrastructure, including a process for the ongoing promulgation of data standards; the status of current standards-setting activities in health data interchange, terminologies, and medical knowledge representation; as well as the need for comprehensive patient safety programs in health care organizations. Recommendations are made for applied research' agenda on patient safety.
This author's investigation was undertaken as part of that process, helping to shed light on the relationships among Nursing Care Hours per Patient Day, patient outcomes, and skill mix. The results of this study highlighted several areas for further research, while raising a number of new Questions. First, the findings suggest the Nursing Care Hours per Patient Day formula may be an ineffective method of staffing nursing units, because it does not address the importance of skill mix, particularly the proportion of Registered Nurses. Indeed, although a higher number of Nursing Care Hours per Patient Day seems beneficial, at first glance, this statistic may represent both a lower proportion of Registered Nurses and unimproved patient outcomes. Second, the analysis of the skill mix and nursing-sensitive Quality indicators demonstrates that the total hours of nursing care are not necessarily associated with adverse patient outcomes. The analysis suggests that adverse patient outcomes may be associated more with the proportion of Registered Nurses than with the total number of hours of care, leaving an important Question un-addressed: How many Registered Nurses are adequate to deliver safe patient care? The nursing-sensitive Quality indicators that were measured in this study support the theory that the proportion of Registered Nurses is a critical element in evaluating patient outcomes, and the results demonstrate that adequate nurse staffing and appropriate skill mix are important factors for consideration on the part of nurse executives and others who make critical staffing decisions. Exactly how these factors affect patient care and the size of the staff and its composition is a matter for further investigation and empirical research.
Although there is widespread concern regarding nurse-to-patient ratios and patient safety, it is important that the nursing profession not rely on mandated nurse-to-patient ratios as the universal solution, although legislation and political agendas on nurse-to-patient ratios throughout the United States are evidence of this trend. Buerhaus warned of the dangers of across-the-board mandated ratios and also suggested that the profession of nursing empirically study nurse-to-patient relationships prior to supporting mandatory minimum staffing levels. California was the first state to mandate staffing ratio legislation. As other states observe and learn from California 's experience, the time is propitious for nursing to monitor and evaluate the changes in staffing mix on an ongoing basis. It is the belief of this researcher that minimum staffing levels do not address the complexities of modern patient care. Credible empirical research to date suggests that the Nursing Care Hours per Patient Day formula alone is insufficient and outdated, and that the current focus on staffing ratios ignores the differences in patients and their nursing care needs.
Finally, nosocomial urinary tract infections and patient satisfaction were shown to have significant correlations with the proportion of Registered Nurses. This is an important finding at a time when other healthcare professions are questioning how nursing interventions affect patient outcomes and the overall quality of patient care. Further research is needed to understand the relationships between pressure ulcers and the proportion of Registered Nurses. This investigation suggests that a larger sample size than the one included here, studied over a longer time frame, may produce more statistically significant results. Statistically significant results may also be achieved if a scale for predicting pressure-ulcer sore risk is employed by the Registered Nurses for one year prior to the data being collected and analyzed.
As economic pressures force the healthcare industry to contain costs while continuing to provide quality care, it is imperative that the nursing profession demonstrate essential contributions that lead to positive patient outcomes. With so much emphasis on patient safety and the quality of care, it is appropriate for nursing to rethink the responsibilities and number of nurses needed to deliver patient care that is both safe and economically viable.
The challenge is finding ways to successfully demonstrate these outcomes in terms of language and definitions that foster and support critical decision-making and that may become nationally accepted indicators, as well as evaluating current practices, such as staffing and skill mix, and studying how they relate to patient outcomes. The nursing profession continues to have difficulty supporting efforts with accurate data that confirm the complicated relationships between nursing services and patient outcomes. It is time for these obstacles to be overcome through comprehensive and multifaceted research efforts.
In the United States today, no single measure or process guides appropriate stafting levels in hospitals and acute-care facilities, and there is no standard for benchmarking critical nurse staffing decisions. Although legislation of nurse-to patient outcomes is one way of staffing hospitals, strong scientific evidence demonstrating the relationships between nursing interventions and patient outcomes remains under-examined. This investigation supports further research to challenge outdated practices, to offer proposals for change, and to point the way to more appropriate and effective nursing paradigms
REFERENCIAS
1. Agency for Health Care Policy and Research. Pressure Ulcers in Adults: Prediction and Prevention. Clinical Practice Guidelines Number 3. 1992 [ Links ]
2. Aiken LH. "More Nurses, Better Patient Outcomes: Why isn't it obvious?" Eff Clin Pract [serial online]. 2001. Available at: http://www.acponline.org/journals/ecp/sepoct01/aiken.htm. Accessed February 5, 2001 [ Links ]
3.American Nurses Association, Network. Nurse Staffing and Patient Outcomes. Washington , DC : American Nurses Publishing; 2000 [ Links ]
4.American Nurses Association President Mary Foley. Testimony of the ANA before the Subcommittee on Labor, Health and Human Services, Education and Related Agencies, Committee on Appropriations, United States Senate, on Patient Safety and Medical Errors. Washington , DC : American Nurses Publishing; 1999. Available at: http://www.ana.org/federal/legi/testimony/1999/iom.htm Accessed April 17, 2000. [ Links ]
5. American Nurses Association, Testimony of the ANA before the sub-committee on Labor, Health and Human Services education and related agencies, United States Senate Appropriations Committee on Patient Safety and Medical Errors. Washington , DC : American Nurses Publishing, 1999. Available at: http://www.ana.org/federal/legis/testimon/1999/iom.htm Accessed April17, 2000 [ Links ]
6. Bergstrom N, Braden B, Kemp M, Ruby E. "Multisite Study of Incidence of Pressure Ulcers and the Relationship between Risk Level, Demographic Characteristics, Diagnoses, and Prescription of Preventive Interventions" J Am Geriatr Soc. 1996; 44: 22-30. [ Links ]
7. . Blegan MA, Goode CS, Reed L. "Nurse Staffing and Patient Outcomes" Nurs Res. 1999;47:43-56. [ Links ]
8. Buerhaus P. "What is the Harm in Imposing Mandatory Hospital Nurse Staffing Regulations?" Nurs Econ. 1997;15:66-72. [ Links ]
9. Ditmyer S, Koepsell B, Branum V, Davis P, Lush MT. "Developing a Nursing Outcomes Measurement Tool" J Nurs Adm. 1998; 28:10-16 [ Links ]
10. Donabedian A. Exploration in Quality Assessment and Monitoring: The Criteria and Standards of Quality. Vol 1 Ann Arbor , Mich : Health Administration Press; 1980. [ Links ]
11. Irvine D, Sidani S, Hall McGillis L. "Unking Outcomes to Nurses' Roles in Health Care" Nurs Econ. 1998; 16:58-64. [ Links ]
12. Jennings-Mowinsky B, Staggers N, Brosch LR. "A Classification Scheme for Outcome Indicators" Image: The Journal of Nursing Scholarship. 1999; 31:381-387 [ Links ]
13. . Uchtig LK, Knauf RA, Milholland D. "Some Impacts on Acute Care Hospitals Outcomes" J Nurs Adm. 1999; 29:25-43 [ Links ]
14. McHugh ML. "Productivity Measurement in Nursing" Ward MJ, Price SA. Issues in Nursing Administration. St. Louis , Mo : Mosby-Year Book; 1989:415-418 [ Links ]
15. Nursing Facts, American Nurses Association. "Nursingsensitive Quality Indicators for Acute Care Settings and ANA's Safety and Quality Initiative." 1999. Available at: http://www.ana.org/readroom/fssafe99.htm Accessed October 7; 2002 [ Links ]
16. Philip Aspden, Janet M. Corrigan, Julie Wolcott, Shari M. Erickson, Editors, Committee on Data Standards for Patient Safety. "Patient Safety: Achieving a New Standard for Care." Washington , DC : Institute of Medicine , National Academy Press; 2003 [ Links ]
17. Seago JA. "The California Experiment: Alternatives for Mínimum Nurse-to-Patient Ratios" J Nurs Adm. 2002; 32: 48-58. [ Links ]
18. Sovie MD. "Tailoring Hospitals for Managed Care and Integrated Health Systems" Nurs Econ. 1995; 13: 72-83. [ Links ]
19. Wunderlich GS, Sloan FA, Davis CK. Nursing Staff in Hospitals and Nursing Homes: Is It Adequate? Washington, DC: Institute of Medicine, National Academy Press; 1996. [ Links ]














