Introduction
Intestinal ostomies consist of surgical openings to exteriorize a segment of the intestine to supply the needs of fecal elimination 1. The process of living with an ostomy has repercussions on biopsychosocial aspects and promotes changes and adaptations in people’s daily habits, self-care, and self-image 2.
Self-care is one of the main factors altered in the life of a person with an ostomy, due to the new demands of body care that permeate aspects such as body hygiene, stoma and peristomal skin, nutrition, sexuality, social relations, and psychological factors. Insufficient self-care can lead to complications associated with the stoma and hinder the adaptive process 3.
Dorothea Orem defines self-care as actions that people perform to maintain the functioning and well-being of the body, preserving organic development, health, and life. When there is an imbalance between the demands and the ability to perform these actions, there is a self-care deficit, a situation in which the nurse plays an important role in supporting the patient who has difficulties in self-care 4.
People with ostomies experience deficits, especially during the initial period after surgery, related to the new skills required in the care of the ostomy and the collection equipment, as well as the psychological and social repercussions 5. These aspects derive from problems of acceptance and aversion to touch or care for the stoma, and from difficulties with the required skills and in the process of learning about self-care 3,6.
Such factors need to be developed and directed by the nurse in the process of health education, in which the person with an ostomy, along with caregivers and family members, has a central and active role. For this, Orem establishes essential actions for the provision of self-care, called “requisites”, which can be universal when they concern the maintenance of life, developmental when related to body changes or new events, and of health deviation when associated with pathologies or injuries 4.
It is fundamental that people with ostomies develop these requisites in their learning process of self-care with the support of nursing, especially because the nurse has an important role in the performance of healthcare services for people with ostomies within the Unified Health System (SUS, by its acronym in Portuguese), participating in the comprehensive assistance to the population, as well as in the duties of organizing services 7.
In this sense, this study is justified by the need to expand the knowledge of nurses about the requisites of self-care, aiming to improve the assistance provided, in addition to giving information that can support the development of technologies and educational methods for the self-care of this population. Therefore, the objective of the study is to map the self-care requisites for people with intestinal ostomies in their adaptive process, guided by Orem’s theory.
Materials and Methodology
The study consists of a scoping review conducted from May to June 2022, based on the theoretical framework of Orem’s selfcare deficit nursing theory 4, in which studies published from 2000 to 2022 were selected. We followed the protocol of the Joanna Briggs Institute (JBI) Reviewers’ Manual: delimitation of the research question, surveys of studies in the literature, selection based on eligibility criteria, data analysis, synthesis, and presentation 8. For the structured presentation of results, the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR [9]) were followed.
A search for protocols similar to this review was performed in April 2022 in the JBI Clinical Online Network of Evidence for Care and Therapeutics (COnNECT+), Database of Abstracts of Reviews of Effects (DARE), The Cochrane Library, and International Prospective Register of Ongoing Systematic Reviews (PROSPE-RO) data sources. It was found that there are no protocols similar to the purpose of this study.
After that, a search protocol was created with the following items: objective, guiding question (mnemonic “Population, Concept, Context - PCC”), inclusion and exclusion criteria, search strategy, data to be extracted from the studies, and form of presentation of results. The study protocol was registered on the Open Science Framework (OSF) platform under the DOI: 10.17605/OSF.IO/XRH5K.
The guiding question was elaborated from the mnemonic “PCC”, in which “P” indicates people with intestinal ostomies; “C”, selfcare requisites; “C”, adaptive process. In this way, the aim is to question what self-care requisites are necessary for people with ostomies in their adaptive process.
The descriptors were selected in the indexed vocabulary of the Medical Subject Headings (MeSH) and Descriptors in Health Sciences (DeCS); in addition, the keywords were searched in the studies available in the National Library of Medicine (PubMed) and the Cumulative Index to Nursing & Allied Health Literature (Cinahl), according to the recommendations of the JBI. Based on this, the following search strategy was elaborated: (ostomy OR colostomy OR ileostomy OR stoma) AND (self-care OR self-management) AND (adaptation OR adjustment).
The following data sources were used: Medical Literature Analysis and Retrieval System Online (Medline), Cinahl, Scopus, Latin American and Caribbean Health Sciences Literature (Lilacs, by its acronym in Portuguese), Nursing Database (BDEnf, by its acronym in Portuguese), Índice Bibliográfico Español en Ciencias de la Salud (IBECS), Web of Science, and Scientific Electronic Library Online (SciELO). Regarding the gray literature sources, studies were sought in the Brazilian Digital Library of Theses and Dissertations (BDTD, by its acronym in Portuguese), the Open Access Scientific Repository of Portugal (RCAAP, by its acronym in Portuguese), Theses Canada, the DART-Europe E-Theses Portal, and the National ETD Portal.
Due to the specifications of the data sources, the search strategy was adapted to each of them, but we tried to keep it as similar as possible to the original strategy. Table 1 presents the strategies used for each source.
Table 1 Search Strategies Conducted in Each Data Source. Natal, Rio Grande do Norte, Brazil, 2022
| Search Strategies | Source |
|---|---|
| TI ostomy OR TI colostomy OR TI ileostomy OR TI stoma AND TI self care OR TI selfmanagement AND TI adaptation OR TI adjustment | Medline |
| TI ostomy OR TI colostomy OR TI ileostomy OR TI stoma AND TI self care OR TI selfmanagement AND TI adaptation OR TI adjustment | Cinahl |
| (TITLE-ABS-KEY (ostomy) OR TITLE-ABS-KEY (colostomy) OR TITLE-ABS-KEY (ileostomy) OR TITLE-ABS-KEY (stoma) AND TITLE-ABS-KEY (self AND care) OR TITLE-ABS-KEY (self AND management) AND TITLE-ABS-KEY (adaptation) OR TITLE-ABS-KEY (adjustment)) | Scopus |
| (tw:(ostomy)) OR (tw:(colostomy)) OR (tw:(ileostomy)) OR (tw:(stoma)) AND (tw:(self-care)) OR (tw:(self-management)) AND (tw:(adaptation)) OR (tw:(adjustment)) | Lilacs |
| (tw:(ostomy)) OR (tw:(colostomy)) OR (tw:(ileostomy)) OR (tw:(stoma)) AND (tw:(self-care)) OR (tw:(self-management)) AND (tw:(adaptation)) OR (tw:(adjustment)) | BDEnf |
| (tw:(ostomy)) OR (tw:(colostomy)) OR (tw:(ileostomy)) OR (tw:(stoma)) AND (tw:(self-care)) OR (tw:(self-management)) AND (tw:(adaptation)) OR (tw:(adjustment)) | IBECS |
| (tw:(ostomy)) OR (tw:(colostomy)) OR (tw:(ileostomy)) OR (tw:(stoma)) AND (tw:(self-care)) OR (tw:(self-management)) AND (tw:(adaptation)) OR (tw:(adjustment)) | SciELO |
| (all fields: ostomy AND all fields: self-care) | BDTD |
| Ostomy OR (colostomy OR ileostomy OR stoma) AND self-care OR (self-management) AND adaptation OR (adjustment) | RCAAP |
| Ostomy OR colostomy OR ileostomy OR stoma AND self-care OR self-management AND adaptation OR adjustment | Theses Canada |
| Ostomy OR colostomy OR ileostomy OR stoma AND self-care OR self-management AND adaptation OR adjustment | DART-Europe E-Theses Portal |
| Ostomy OR (colostomy OR ileostomy OR stoma) AND self-care OR (self-management) AND adaptation OR (adjustment) | National ETD Portal |
Source: Elaborated by the authors.
The eligibility criteria included studies that presented at least one requisite of self-care (actions aimed at the provision of selfcare [4]) for people with intestinal ostomies, whether or not they addressed Orem’s theory, and that were published in full online in the Journals Portal of the Coordination for the Improvement of Higher Education Personnel (Capes, by its acronym in Portuguese). Access to the portal was through the Federated Academic Community (CAFe, by its acronym in Portuguese), a resource funded by the university where the study was conducted. Duplicates, editorials, experience reports, opinion articles, and theoretical essays were excluded.
The studies were initially selected based on the titles and abstracts, and after the initial sorting, they were read in full for the sample selection. The search was conducted by two researchers independently, and at the end, the selected texts were compared and read in their entirety. In case of disagreement, a third researcher delimited the study to be included. No software was used in the process of selection and analysis of the studies.
The self-care requisites were grouped as proposed by Orem 5: universal when they addressed basic activities of daily living for the functioning of the body, developmental when related to specialized actions of the universal requisites for changes in body development or new conditions or events, and health deviation for situations of diseases or injuries that require diagnostic, therapeutic or rehabilitative care actions. Moreover, the requisites were subdivided into thematic categories based on the Brazilian Consensus on Stomal Therapy 10.
The selected studies were identified by the letter “E”, from E1E83 6,11-96. The data extracted from the studies of the final sample (identification data, type of study, and recommendations for self-care) were tabulated in a Microsoft Excel spreadsheet, analyzed according to descriptive statistics, and presented in table format.
Results
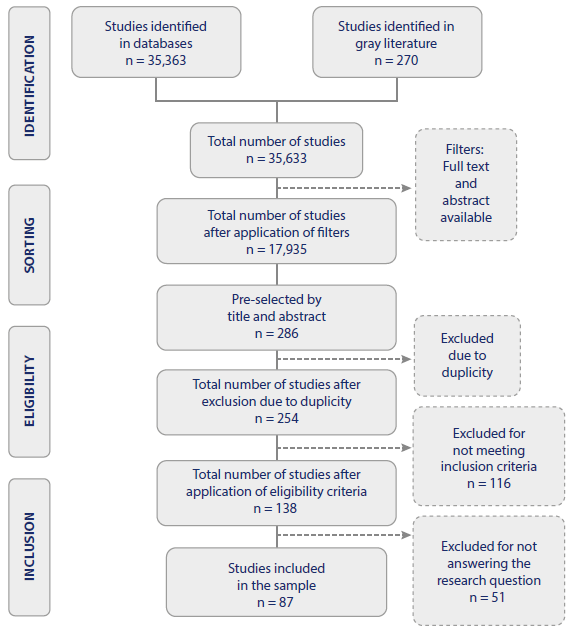
A total of 35,363 studies were identified in the databases and gray literature, of which 87 were selected to compose the sample, as detailed in the diagram of Figure 1. Of this total, 78 are articles, with eight dissertations and one thesis.
Regarding the characterization of the studies in the sample, it was found that most were from the Cinahl database (52; 59.8%) and the British Journal of Nursing (18; 20.7%), published in the United Kingdom (40; 46.0%) and carried out in the United Kingdom (44; 50.6%). The publications occurred between 2000 and 2022, mostly in the years 2019 (9; 10.3%), 2013 (8; 9.2%), and 2014 (7; 8.0%), and were found to be predominantly literature reviews (50; 57.5%). Regarding self-care requisites, 78 requisites were identified, of which 19 were classified as universal, 41 as developmental, and 18 as health deviation.
Concerning the universal requisites, described in Table 2, most studies were identified in the category “nutritional aspects”, of which the most frequent was “eating regularly and following a balanced diet”. In addition, within this category, the least frequent were “observe the effects of dietary changes on stool” (5; 5.7% [29,36,73,78,92]), “avoid consuming large amounts of fluid during or immediately before or after meals” (4; 4.6% [14,22,32,34]), “avoid talking while eating” (3; 3.4% [56,75,78]), “avoid foods that may cause obstruction” (3; 3.4% [16,21,73]), “avoid foods that cause diarrhea” (3; 3.4% [14,15,52]), and “control foods that cause odor” (2; 2.3% [18,78]).
Source: Elaborated by the authors.
Figure 1 Diagram of Study Selection from Data Sources. Natal, Rio Grande do Norte, Brazil, 2022
Table 2 Absolute and Relative Frequency of the Universal Requisites Identified in the Studies. Natal, Rio Grande do Norte, Brazil, 2022
| Universal requisites | Studies | n (%) |
|---|---|---|
| Nutritional aspects | ||
| Eat regularly and follow a balanced diet | E2, E6, E12, E13, E15, E16, E17, E18, E19, E20, E23, E27, E29, E33, E40, E46, E48, E49, E67, E69, E71, E75, E84. | 23 (26.4) |
| Maintain a good fluid intake | E2, E4, E8, E9, E17, E19, E20, E24, E27, E33, E40, E46, E48, E49, E51, E56, E67, E69. | 18 (20.7) |
| Avoid gas-producing foods | E2, E12, E13, E15, E17, E51, E56, E63, E67, E69, E71, E80, E81, E82. | 14 (16.1) |
| Masticate food thoroughly | E2, E12, E17, E19, E27, E33, E37, E40, E46, E48, E56, E67, E69, E71. | 14 (16.1) |
| Taste foods gradually | E12, E17, E20, E23, E24, E27, E33, E40, E56, E69, E71. | 11 (12.6) |
| Intestinal control | ||
| Watch for signs of change in the stool | E5, E7, E37, E45, E53, E63, E86. | 7 (8.0) |
| Physical activities | ||
| Perform moderate physical exercises to prevent constipation | E19, E20, E39, E51. | 4 (4.6) |
| Take walks to help stimulate bowel function and muscle tone | E39, E40, E62. | 3 (3.4) |
| Professional clinical advice should be sought before beginning any kind of exercise | E39, E40. | 2 (2.3) |
| Sexuality | ||
| Express concerns and doubts about sexual aspects and body image | E66, E73, E75, E84. | 4 (4.6) |
| Explore other comfortable positions for sexual activities | E66, E73, E83. | 3 (3.4) |
| Accept to adapt to changes and self-image after the ostomy | E85, E87. | 2 (2.3) |
| Discuss aspects that can improve self-image with health-care professionals | E36. | 1 (1.1) |
Source: Elaborated by the authors.
As for the developmental requisites, described in Table 3, the predominance of the category “stoma and peristomal skin care” and the requisite “assess peristomal skin integrity” were observed. In this category, the least frequent requisites were “keep the peristomal skin clean and dry” (4; 4.6% [43,46,67,74]), “cut the peristomal skin hairs” (3; 3.4% [45,79,83]), “measure the length and width of irregular stomas” (2; 2.3% [45,63]), and “expose the skin around the stoma to the sun” and “protect the stoma with moist gauze” (1; 1.1% [83]).
Table 3 Absolute and Relative Frequency of the Developmental Requisites Identified in the Studies. Natal, Rio Grande do Norte, Brazil, 2022
| Developmental Requisites | Studies | n (%) |
|---|---|---|
| Stoma and Peristomal Skin Care | ||
| Assess peristomal skin integrity | E20, E26, E23, E25, E29, E32, E33, E35, E37, E38, E40, E43, E46, E47, E50, E52, E53, E54, E55, E56, E58, E67, E68, E69, E72, E76, E86. | 27 (31.0) |
| Clean the peristomal skin with tap water and dry thoroughly | E1, E9, E15, E17, E19, E21, E22, E25, E26, E29, E38, E40, E41, E56, E57, E58, E67, E69, E72, E76, E81, E82. | 22 (25.3) |
| Check the normal appearance of the stoma | E3, E4, E7, E9, E15, E17, E20, E24, E27, E29, E40, E41, E43, E46, E50, E52, E67, E72, E76, E77. | 20 (23.0) |
| Assess the viability of the ostomy and its characteristics | E7, E8, E25, E29, E35, E38, E50, E52, E55, E68, E72, E76. | 12 (13.8) |
| Avoid the use of moisturizers on the peristomal skin | E29, E41, E56, E58, E68, E69, E76. | 7 (8.0) |
| Choice of Collection Equipment and Supplies | ||
| The opening of the base plate should be cut in the diameter of the stoma | E1, E3, E7, E8, E13, E14, E17, E20, E24, E29, E38, E40, E41, E50, E58, E61, E68, E72, E76, E77. | 20 (23.0) |
| Use products that act as a barrier to protect the peristomal skin | E3, E8, E17, E19, E21, E24, E26, E32, E38, E44, E46, E47, E50, E57, E58, E65, E68, E69, E72. | 19 (21.8) |
| Remove the collection bag carefully | E1, E3, E15, E17, E21, E22, E25, E38, E57, E58, E67, E69, E72, E76, E77. | 15 (17.2) |
| Measure the stoma to define the size of the collection bag cutout | E15, E17, E23, E24, E25, E29, E38, E40, E56, E61, E67, E76, E77. | 13 (14.9) |
| Empty the bag when it is 1/3 or even 1/2 full | E1, E3, E7, E9, E17, E29, E33, E40, E56, E69, E72, E76. | 12 (13.8) |
| Choice of Collection Equipment and Supplies | ||
| Choose the collection equipment according to the needs, individual characteristics, and type of stoma | E10, E11, E12, E22, E23, E37, E41, E52, E68, E69, E72, E76, E85. | 13 (14.9) |
| Use products for stomas to fill skin folds and level the skin | E3, E8, E19, E32, E38, E40, E41, E44, E50, E60, E72. | 11 (12.6) |
| Use bags with activated charcoal filters for the neutralization of odor | E12, E17, E51, E56, E67, E69, E71, E74, E77, E78. | 10 (12.0) |
| Use a transparent collection bag when it is necessary to visualize the stoma | E4, E7, E12, E41, E72, E77. | 6 (6.9) |
| Use deodorant sprays in the bag to control odors | E27, E44, E51, E56, E69, E71. | 6 (6.9) |
| Nutritional Aspects | ||
| Decrease fiber intake for people with ileostomies | E2, E12, E24, E27, E31, E33, E43, E49. | 8 (9.2) |
| Developmental Requisites | Studies | n (%) |
| Maintain adequate fiber food and fluid intake for people with colostomies | E24, E46, E48, E51, E63, E69. | 6 (6.9) |
| Recognize symptoms of dehydration in people with ileostomies | E2, E30, E59, E67. | 4 (4.6) |
| Sexuality | ||
| Use alternative strategies such as underwear and belts to encourage intimacy | E6, E37, E62, E66, E73, E75, E83. | 7 (8.0) |
| Empty or replace the collection bag before intercourse | E6, E64, E66, E73, E75. | 5 (5.7) |
| Avoid foods that can cause gas or strong odors before intercourse | E66, E75. | 2 (2.3) |
| Clinical Assistance | ||
| Express concerns or anxieties in conversations with health-care professionals | E36, E37, E40, E64, E70, E73, E75, | 6 (6.9) |
| Seek help from professionals to evaluate the possibility of using continence systems | E6, E64, E75, | 3 (3.4) |
| Social Aspects | ||
| Participate in groups with other people with ostomies | E23, E74, E86, E87. | 4 (4.6) |
| Physical Activities | ||
| Empty the collection bag before physical activities | E67, E76. | 2 (2.3) |
Source: Elaborated by the authors.
In the category “care of the collection equipment and supplies”, it was observed that “assess peristomal skin integrity” was the most common requisite. The least frequent requisites were “carefully remove adhesive parts of the collection equipment” (10; 12.0% [25,28,40,41,43,46,50,71,75,77]), “check for signs of leakage in the collection equipment” (9; 10.3% [20,25,27,33,43,47,60,74,79]), “adjust the opening of the collection equipment in the first weeks after surgery” (7; 8.0% [29,45,47,51,74,79,92]), “carefully place the collection equipment around the stoma” (6; 6.9 % [16,24,25,73,83,84]), “take extra supplies and collection equipment when away from home” (6; 6.9% [6,15,75,83,86,87]), “fix the collection equipment correctly from bottom to top on the peristomal skin” (6; 6.9% [11,27,33,41,83,84]), “identify and perform the change of the collection equipment when the plate is saturated” (5; 5.7% [18,44,67,75,83]), “when changing the collection equipment, keep it pressed for a few seconds” (4; 4.6% [26,41,83,84]), “apply the barrier cream in circular movements with the fingertip” (3; 3.4% [28,51,62]), and “monitor the adaptation to the collection equipment” (2; 2.3% [93,95]).
The category “choice of the collection equipment and supplies” had the most common requisite for choosing the collection equipment according to the needs, individual characteristics, and type of stoma. And the requisite “patients along with the nurse select the appropriate collection equipment” was the least frequent (3; 3.4% [25,54,83]).
Table 4 presents the health deviation requisites, which had “choice of collection equipment and supplies” as the most frequent category, and the requisite “use hydrocolloid powder to absorb moisture in cases of dermatitis”. In this category, the least frequent requisites were “change the collection equipment in case of allergic dermatitis” (8; 9.2% [17,21,25,46,58,58,67,71,77]), “use barrier products and rings in the presence of granulomas” (6; 6.9% [25,43,58,69,71, 88]), and “use Aloe vera may help in the management of peristomal complications” (1; 1.1% [30]).
Table 4 Absolute and Relative Frequency of Health Deviation Requisites Identified in the Studies. Natal, Rio Grande do Norte, Brazil, 2022
| Health Deviation Requisites | Studies | n (%) |
|---|---|---|
| Choice of Collection Equipment and Supplies | ||
| Use hydrocolloid powder to absorb moisture in cases of dermatitis | E8, E13, E19, E24, E26, E32, E41, E50, E57, E60, E65, E68, E69. | 13 (14.9) |
| Managing contact dermatitis treatment using ostomy skin barriers | E7, E20, E26, E37, E38, E40, E42, E50, E54, E61, E65, E69. | 12 (13.8) |
| Use a bag with convex barrier rings in cases of retraction | E7, E8, E16, E23, E34, E37, E53, E63, E65, E69, E72. | 10 (12.0) |
| Manage the parastomal hernia with the use of a support belt, one-piece systems, and skin protection products | E1, E5, E7, E20, E23, E46, E53, E63, E65, E69. | 10 (12.0) |
| Identify and manage the underlying cause of stomal complications | E23, E32, E38, E46, E53, E57, E61, E68, E69, E84, E85. | 11 (12.6) |
| Stoma and Peristomal Skin Care | ||
| Monitor the extent of necrosis, assessing the stoma and peristomal skin | E4, E23, E37, E40, E65, E69. | 6 (6.9) |
| Observe signs of ischemia when the stoma presents stenosis | E4, E7, E20, E53, E63. | 5 (5.7) |
| Observe signs of stoma obstruction in case of complications | E5, E86. | 2 (2.3) |
| Prevent stomal and peristomal complications | E85, E86. | 2 (2.3) |
| Demonstrate strategies for the resolution of stomal and peristomal complications | E86. | 1 (1.1) |
| Clinical Assistance | ||
| Seek nursing professional help in case of stomal and peristomal complications | E46, E52, E56, E67, E68, E72, E76, E86, E87. | 9 (10.3) |
| Seek professional help when effluents are above normal volume | E30, E56, E67, E86. | 4 (4.6) |
| Health Deviation Requisites | Studies | n (%) |
| Nutritional Aspects | ||
| Use oral rehydration in case of large losses of fecal content | E59, E67. | 2 (2.3) |
| Physical Activities | ||
| Discontinue exercise in case of health problems | E39. | 1 (1.1) |
| Sexuality | ||
| Seek professional help to evaluate physiological problems related to sexual activities | E6, E62, E64, E66, E73. | 5 (5.7) |
Source: Elaborated by the authors.
Discussion
It was observed that the studies mapped mainly requisites on aspects of care with the stoma and the peristomal skin, nutritional aspects, and the choice of collection equipment and supplies. Moreover, most of the requisites were developmental, related to the changes that people with ostomies face both in body aspects and in activities of daily living. Such findings indicate the need for professionals to emphasize these aspects in the process of health education.
The universal requisites presented the nutritional aspects as the most frequent category, with requisites that addressed proper nutrition, fluid intake, and bowel control, including the observation of changes in the stool. Orem establishes the provision of sufficient food for the needs of body integrity, as well as the care related to elimination needs as essential for self-care. This principle should be considered by nursing, which should support this process so that the individual can manage food choices and control excrement 4.
Given this need, it becomes essential to monitor the changes in eating habits that people with intestinal ostomies experience since nutrition influences bowel function and elimination, which can generate undesirable effects, such as the increase of flatus, associated with the stoma type 97,98, resulting in poorer quality of life, since the loss of consumption of certain foods may deprive the pleasurable sensations associated with eating 99,100.
In this sense, it is necessary that, in this population’s assistance, the orientations about nutritional aspects are included, as well as the available strategies that can help the person in their autonomy, such as the practice of irrigation, if the individual meets the conditions required to perform it 98. Furthermore, the joint work of nursing with the multi-professional team is highlighted, through the services of attention to the health of the person with an ostomy, which has, in the scope of SUS, multi-professional assistance that includes nutritionists to meet the needs of nutritional and dietary assessment 7.
Regarding the developmental requisites, the predominant category was “stoma and peristomal skin care”, with emphasis and more frequency on the requisite “assessment of peristomal skin integrity”, followed by the categories “care and choice of the collection equipment and supplies”, which presented requisites on the correct use and handling of this equipment and the choice of products for self-care. These results are related to the changes experienced and the new self-care needs, which require specific actions for the proper functioning of the ostomy and the protection against complications, in which the support of the nursing team is of fundamental importance.
For this reason, the assessment of the peristomal skin integrity is one of the essential care after having an ostomy, to prevent complications associated with the use of the collection system and the contact of stool with the skin 25. The latest recommendations encourage nurses to enable the patient to assess their stoma and peristomal skin, so that they can actively participate in the care and identify changes for preventive care, with the support of health professionals 10.
Among the factors that can interfere with the integrity of the peristomal skin, the inadequate handling of collection equipment, effluent leakage, and the self-care deficit related to hygiene are highlighted 3. These difficulties occur mainly during the initial period after surgery, which generates feelings of anxiety and insecurity. Therefore, adequate instruction about this care provides greater safety and satisfaction to this population, especially when performed by nurses with specialized knowledge in stomal therapy 101.
Regarding the requisites related to the collection equipment, we emphasize the importance of the choice of the collection equipment being made in a participative way between nurses and the population with an ostomy. In the context of the SUS, the collection equipment and supplies are made available in the care services for people with ostomies free of charge, and when selected appropriately and periodically reassessed, they provide confidence and satisfaction to the person with an ostomy 102, besides contributing to the resolution of complications 7.
The selection of the collection equipment follows the nurse’s prescription, which must be based on the individuality of each person, considering the aspects of the patient’s preference, type of ostomy, adaptation, peristomal skin, and characteristics of the person’s abdomen 10.
As for the health deviation requisites, the main category referred to the choice of the collection equipment and supplies, in which the main requisite dealt with the use of hydrocolloid powder to absorb moisture in cases of dermatitis. This category, as well as that of stoma and peristomal skin care, indicated mainly the handling of stomal and peristomal complications, present in several studies.
Complications, besides negatively impacting the adaptation of people with ostomies, cause costly expenses for health services. Thus, the population can benefit from more emphasis on preventive education rather than only receiving curative treatment 103.
Several products are available to assist in the prevention and treatment of stomal and peristomal complications, such as barrier films, adhesive removers, pastes, and powders with actives that protect or assist in the healing of lesions. It is necessary to assess not only the lesion but also the person with an ostomy as a whole, given the impact that this complication can cause in their lives, to then designate a specific conduct for each situation 104.
Regarding the categories of physical activities, sexuality, and social aspects present in the requisites, this review highlights the scarcity of research on these topics. This can be explained because, in self-care, the emphasis is notoriously on practical skills related to ostomy care, along with the peristomal skin and the collection equipment.
However, the repercussions of an ostomy transcend the physiological changes and alter how the person sees him or herself and how he or she relates to other people as a result 105. According to Orem, health deviation requisites also encompass the need to accept self-image modifications arising from treatments, health conditions, or illness 4. Thus, a multidimensional nursing approach that focuses, in addition to physical changes, on emotional, sexual, and social aspects is imperative to assist in the self-care of this population.
It is also noteworthy that self-care involves not only the practical care with the ostomy and the collection equipment, but also the psychological, physical, and environmental needs 4. Thus, sensitivity and knowledge of nursing are crucial to identifying the main needs of this population, in an individualized and holistic way, to provide the demands of self-care.
Some strategies and educational technologies are being produced and have shown positive effects on health education, which can support nursing care to the person with an ostomy for the provision of self-care 106. Considering the requisites identified in this study, it is expected to assist in the planning of interventions for the self-care of this population, as well as in new studies for the advancement of knowledge in the area.
As a limitation, this review presents the mapping of the requisites identified in different types of studies without assessing the degree of evidence and indication for clinical practice. More studies are needed to understand these requisites based on the experiences of people with ostomies and evidence-based research, using Orem’s theory to support nursing care for this population.
Conclusions
This study presented the main self-care requisites mapped in the literature and guided by Orem’s theory. The universal requisites mainly addressed nutritional aspects; for the developmental requisites, the stoma and peristomal skin care predominated; as for the main health deviation requisites, they dealt with the choice of the collection equipment and supplies in case of complications. Few studies addressed the categories “physical activities”, “sexuality”, and “social aspects.”
Therefore, the requisites identified in this study can guide nursing care to the person with an ostomy, improving the assistance provided and the process of learning self-care. Furthermore, the study contributes to the advancement of nursing as a science by presenting the mapping of evidence based on a nursing theory. New intervention studies and the development of technologies based on the results of this review are suggested.















