Introduction
The demographic and epidemiological transition has allowed an increase in life expectancy worldwide 1; therefore, living with more than one Chronic Non-Communicable Disease (CNCD) 2 such as arterial hypertension, Type II diabetes, dyslipidemias, and heart diseases, which are risk factors to develop a stroke, requires greater demand of constant health care measures in older adults (OAs) 3.
Stroke causes neurological lesions due to the reduction or interruption in blood supply that feeds oxygen and nutrients to the brain, generating cell death 3. According to its etiology, the mean incidence of stroke is 200 cases for every 100,000 inhabitants per year; in addition, it is worth noting that 17.9 million people died due to stroke in 2019, which represents 32 % of all deaths in the world 4.
It is worth noting that strokes are the leading cause of death among people aged from 40 to 70 years old, accounting for four out of five deaths worldwide 4. The Mexican Health Department reported that 37,453 people died in 2021 5, of which 18,843 were men aged 65 years old; in addition, 118 cases for every 100,000 inhabitants are estimated per year, that is 170,000 new cases 6, from which seven out of ten remain with some disability 7.
Given this fact, it is estimated that by 2050, when almost half of the Mexican population will be over 60 years old, 50 % of hospital admissions will be related to cardiovascular problems, and the survivors will have severe physical and cognitive lesions 7 that generate disability-adjusted life years and years lived with disability, which interact unfavorably with OAs’ intrinsic capacity and result in their total dependence 8.
There are approximately 100 million stroke survivors in the world and more than one-third of them live with some disability and dependence level 9,10; for this reason, there is an imminent need for family caregivers (FCs) to assume responsibility for home-based care to meet the basic needs of daily life, in addition to those related to the specific care regarding the physical or cognitive disabilities imposed by the stroke 11.
FCs are individuals that belong to the family nucleus, aged over 18 years old and in charge of providing care and physical, emotional, and spiritual assistance to disabled and dependent OAs, either in the hospital or at the home environment; they are also the people making decisions and assuming self-care 12-14.
Being an FC changes and impacts life in the physical, emotional, social, and spiritual dimensions, positively or negatively, given the inherent complexity during the transition to and adoption of the caregiver role, which is why it is necessary that FCs express their underlying uncertainty in the face of lack of knowledge and care management during this transition 15.
Unpreparedness and lack of care skills 16,17 hinder the transition to adopt the caregiver role 18,19. Various sources point out that FCs describe care as a complex task that generates stress and physical and mental exhaustion, given the uncertainty about eventual complications that may arise while providing care 20,21. This situation generates feelings of impotence and incompetence that result in anxiety, fear, and anguish related to hospital discharge 22; however, the role can be learned 15 and confidence in its adoption can be fostered from Nursing therapeutic education 23,24.
Currently, the development and use of theories about specific situations in the care practice have contributed to increasing and irreversible advances in the Nursing science, based on Middle-Range Theories (MRTs) that describe, explain, and predict the phenomenon of interest for Nursing to properly select an approach, use it, modify it and apply it to patients, families and communities, as the theories have a pragmatic meaning 25.
Currently, MRTs are a key model for developing Situation-Specific Theories (SSTs) with certain theoretical, methodological and empirical subtraction levels and which favor both practice and research 26, as they coherently describe various concepts related to the naturalness of the phenomena at a present moment, in addition to providing a logical explanation for the relationship, interaction and prediction of results among the concepts 27.
In other words, SSTs are characterized as being less abstract and complex, which eases their verification and application in real-life situations. These theories allow an orderly and systematized articulation of the elements generated from the theorization processes; they also incorporate specific diversities and complexities of each situation and ease the transformation of the knowledge generated through theorizations that guide the essential actions using research concepts and constructs 27.
Given the aforementioned, although some MRTs and SSTs can be applied to the context of our study phenomenon, they fail to fully describe the reality of the phenomenon in our target population. It is important to consider that CNCDs encompass a wide range of conditions, each one with its own complexity level. In the case of FCs of disabled and dependent individuals due to stroke, they face multiple needs that include disease management, psychological support, coping and adaptation, education, support for decision-making and personal care. It is crucial to recognize and address these needs to ensure well-being, both for the caregiver and for the patient.
Considering the complexity inherent to the phenomenon of interest, it is necessary to develop an SST to better understand the experience of FCs of OAs who have suffered a stroke. The description above will provide a guide for the clinical practice in real-life situations, improve research in the field and contribute to theoretical and scientific progress in the scope of the care offered to stroke patients. This will foster theoretical expansion in the Nursing discipline and strengthen its knowledge base.
There is an urgent need to generate new information from SSTs in the Nursing discipline, due to the difficulties faced by researchers to transform the concepts from the main theories into practical knowledge that can be applied to care. The methodology proposed by Afaf Meleis and Im offers a more fluid integrating process that is reflected in health care professionals’ everyday performance.
This methodology addresses the complexity and diversity inherent to care situations, providing a practical and applicable approach centered on the reality and specific needs of patients and health professionals, which is why greater relevance and effectiveness are achieved in clinical practice.
In this sense, SSTs are characterized by their applicability and verification ease in real-life situations. Meleis and Im’s methodological proposal offers an integrating and fluid approach that reflects health care professionals’ everyday practice, addressing the difficulty of transforming theoretical concepts into practical and applicable knowledge and allowing for a better adaptation to the individual needs and evidence-based good quality care in the Nursing field. Likewise, one of the characteristics of SSTs is that they do not intend to be universal, as they are dynamic and variable over time 27. Considering these premises, the objective of the current paper was to develop an SST proposal about the transition to the role of FC of OAs after a stroke, based on the integrating approach proposed by Afaf Meleis and Im.
Methodology
The SST developed from the integrating approach proposed by Afaf Meleis and Im 27-29 resorts to two reasoning strands, as it combines and associates different data sources. These sources can be an already existing SST, previous research studies or perceptions suggested by the practice. Integrating these processes leads to the creation of new theorizations. The SST integrating approach takes place through five different stages, which are grounded on principles that guide the development of conceptualizations and theorizations 27. These stages are described in detail below.
The first step has to do with the context and the population: It consists in exploring and thoroughly understanding the phenomenon of interest, considering the specific environment where it arises and the particular characteristics of the population involved. This implies considering the social, cultural, economic, and political contexts, as well as the demographic characteristics, needs, and experiences of the population affected 27.
When exploring the phenomenon, according to the context, the intention is to understand how the environment where it arises can influence its onset, development, and consequences, which implies examining the influences and contextual factors that may be present and play a role in understanding and explaining it 27. On the other hand, when exploring the phenomenon according to the population, the objective is to understand how the specific characteristics of the population affected can influence its manifestation and experience, which includes considering variables such as age, gender, ethnicity, socioeconomic status and any other demographic or individual characteristic that may exert an impact on its understanding and approach 27.
The second step implies carefully examining the assumptions of the study phenomenon in the light of the proposals outlined in the Fundamental Theory (FT) that sustains the development of the SST. This encompasses an exhaustive analysis of the philosophical contributions that give rise to ontological, epistemological, logical and ethical dimensions. The objective is to understand the diversity and scope of knowledge, both internal and external to the study phenomenon. If these assumptions are in line with the principles of multiple truths, evolutionary capacity in theoretical development and sociopolitical contextualization of phenomena, as well as with the Nursing perspectives, then the concept of creating an SST can be considered valid 27.
The third stage implies exploring the phenomenon from different sources to derive theorizations. It is essential to examine the already existing theories in the Nursing field since, according to Meleis, the development of an SST should strengthen Nursing as a science. Therefore, elaboration of the SST should be based on the Nursing discipline itself, its practice, and its mastery and perspective 27.
Development of an SST is based on deduction from an already existing theory to obtain explanations or predictions about phenomena, situations, or specific populations, resorting to explanations or predictions previously described in theoretical structures. Deductive reasoning plays an important role in conceptualization, as it allows deriving the structure of a supporting theory that sustains the reconsiderations related to the phenomenon under study 27.
Other sources are used inductively for this purpose, such as literature reviews, which provide an expanded understanding of the existing knowledge about the phenomenon and contribute important elements to guide the development, modification, definition or refinement of concepts, assumptions and proposals derived from the supporting theory 27.
The fourth stage in developing an SST is called “Theorization” and is divided into Initialization, Process, and Integration. The initialization phase signals the starting point from where the first theorization emerges, which can originate from various data sources such as literature reviews about the phenomenon of interest, research projects, practical experience or supporting theories that derive concepts and assertions that are relevant to the specific situation 27.
The data obtained from various sources are integrated through the researcher’s reflexive ability, data analysis and the creation of structures that allow formulating proposals. This process can be eased and refined using dialog exchanges, both internal and external to the environment where researchers conduct their research or experience extension or teaching clinical situations 27.
The last stage encompasses verifying and validating the conceptual elements; here, the manuscript is presented, and the theorization is shared in research model or report format with the Nursing academic community 27. The main objective is to obtain due validation by experts through review and criticism. Likewise, the theory needs to be validated by those involved, that is, the specific population group so that they assess its social relevance and usefulness. The integrality of the five stages is shown in Figure 1, as the integrating strategy stems from the veracity of “multiple truths” as an essential assumption to develop SSTs in Nursing 27, considering that another theoretical premise states that “development of the theory is a dynamic and clinical process that changes over time in various contexts” 28. Considering the aforementioned, the current SST derives from an integrating approach between research and practice in the light of the MRT of transitions. The adaptation to each step as proposed in the development of the current SST is briefly described below.
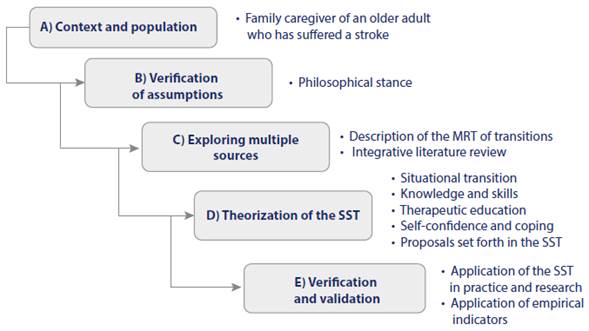
Source: Prepared by the authors based on the steps proposed by Meleis and Im 27
Figure 1 Steps to Develop the Situation-Specific Theory: Transition to the Role of Caregiver of Older Adults after a Stroke
Results
In response to the methodology selected, the main results corresponding to each of the stages described above are presented.
Step A) Context and population
The demographic characteristics of FCs in Mexico are as follows: more than 67 % to 90 % are the OAs’ sons or daughters (3033), with a mean age between 36 and 45 years old 30,31,33. It is worth noting that 22.3 % are also OAs performing the FC role 33, that most of them are devoted to household chores 32,33 and that 66.1 % have Elementary or High School (30, 31); in turn, 73.1 % profess the Catholic doctrine and 73.1 % state having no degenerative chronic diseases 33; finally, all the family members assume the caregiver role according to their schooling level and social and cultural pressure and devote between 9 and 17 hours a day to caring for disabled and dependent OAs 31,33. These data are similar to those from some Latin American countries; in this sense, FCs of OAS with some disability and dependence degree after a stroke are sons/daughters or spouses aged between 18 and 78 years old 34-38. Most of the FCs mention schooling levels from 6 to 12 years of study and their schooling is unfinished in some cases, with socioeconomic levels from average to low in the dyad 35,36,39.
The literature indicates that, in countries with low economic resources, the conditioning factors for the health status of FCs of dependent chronic patients are sedentary lifestyle, overweight, systemic arterial hypertension, Type II diabetes, musculoskeletal deterioration and pain as main health conditions 37,40 that interfere in the transition to adopting the caregiver role.
Afaf Meleis defines transition as a period that begins with the first hints of change anticipation, perception or manifestation. Instability, confusion and stress are experienced during this stage. The transition culminates in an “end” that signals a new beginning or a stability period 41.
In other words, it is a complex and multidimensional process that involves changes in people’s lives, from known and familiar situations to others that are new and unknown. According to Meleis, there can be different types of transitions: 1) health-disease transitions, 2) role transitions, or 3) transitions in life development 42. The theorist highlights that transitions imply adjusting and adapting to new roles, responsibilities and environments, in addition to not only exerting impacts on personal life but also on the family, social and cultural contexts where they take place 43.
Given the above, it is of utmost importance to understand the transition to the role of FC of a disabled and dependent patient after a stroke. Such transition refers to the process by means a family member assumes the responsibility of caring for a loved one who has suffered a stroke, which is a long-term chronic condition. This process implies a significant change in the person’s roles and responsibilities, as well as in their everyday routine and the dynamics of their relationship with the patient.
During this transition, FCs face challenges such as the following: learning about the disease, managing the patients’ symptoms and medications, coordinating medical appointments, providing emotional and social support, and making care-related decisions. It can also imply changes in the family dynamics, redistribution of roles, and adaptation to new routines and requirements.
It is important to note that the transition to the FC role can be emotionally and physically exhausting. Caregivers can experience care burden 34,38, fair health status perception 40,44, stress, anxiety, loneliness and depression 34,38,45, insomnia 32,46 or uncertainty and even fear of delegating care due to the radical change they are undergoing 47.
The psychoemotional perceptions already described arise from the concern about not knowing how to provide suitable care 48, starting from the fact that the person lacks the necessary knowledge and skills to provide home-based care 49; in this sense, it is necessary that Nursing professionals offer multidisciplinary interventions to generate care-related knowledge and skills 44, considering that care skills are a protective resource that develops self-confidence and coping 47.
It is essential to provide FCs with suitable support and resources, including education, training, counseling and access to community support networks to help them cope with this transition healthily and effectively. By providing these resources, self-confidence and adequate management of the situation will be fostered. In addition, it is sought that caregiver can play their role effectively when providing hood quality home-based care, paying attention to hygiene, feeding, medications, comfort and rehabilitation in the case of disabled and dependent people after a stroke.
It is important to highlight that healthy adoption of the caregiver role implies assuming the responsibility of assisting another person in a balanced and conscious way, considering both the patients’ well-being and their own. This implies performing self-care practices that define the suitable limits, searching for emotional, physical, and spiritual support when necessary, and acquiring knowledge and skills to offer proper care, using the resources and services available for the care recipients to be able to better adapt to the environment 50. On the other hand, adopting a pathological stance in this role shows an inability to properly perform this function and to seek help that guides the care to be provided 50. The consequence is an ineffective transition that results in complications such as stress, anxiety, loneliness, depression 34,38,45 and insomnia 32,46.
In this sense, Parada et al.45 found that loneliness, depression, and anxiety (p<0.05) lead to a reduction in adoption of the caregiver role. Therefore, it is necessary to develop interventions targeted at improving the transition in a healthy way among these caregivers of OAs with post-stroke sequelae 50.
Step B) Verification of Assumptions to Develop the Theory
The following assumptions emerge from the philosophical perspective of the Theory of Transitions:
The first assumption sets forth that the situational transition to the role of FC of OAs affected by a stroke is a sudden process that generates a change in the basic life patterns. This situation generates feelings of anxiety, concern, uncertainty, fear and depression in FCs as a result of the diagnosis, disability and care complexity, as caregivers are not prepared to assume this new role 51-54.
The second assumption indicates that a lack of care-related knowledge and skills in FCs of OAs affected by a stroke can hinder a healthy transition to adopting the role. Ineffective or pathological transitions can cause changes in the relationships, skills and behavioral patterns that affect the development of self-confidence and coping in the caregiver 53-55.
The third assumption highlights that the development of self- confidence and coping is characterized by the adoption of the role of caregiver of the OA affected by a stroke on the part of the FC, who is aware of the importance of his/her role as a care provider. In addition, caregivers offer support to the multidisciplinary health system for care continuity at home, which allows self-management of the dyad (patient and caregiver) and favors a healthy transition in adopting the role 55-58.
The fourth assumption refers to Nursing therapeutic education, whose objective is to provide FCs with educational interventions along with the multidisciplinary team and focused on the specific problem. Considering that nurses are the main caregivers of people undergoing transitions, it is important to intervene to favor lower care complexity and improve the transition, which allows the development of self-confidence and coping in adopting the role of caregiver of people affected by a stroke 58-60.
Step C) Exploration through multiple sources
For the development of the SST, Meleis and Im propose generating knowledge in the light of an FT, with the purpose of not losing the essence of the discipline and avoiding distortions, in addition to a literature review along with practical experience 27-29. According to these premises, the philosophical grounds of the current SST lie in Afaf Meleis’ Theory of Transitions and are guided by the empirical evidence found in multiple databases.
Description of Afaf Meleis’ Middle-Range Theory of Transitions
The conceptual description of the current SST derives from Afaf Meléis’ Theory of Transitions, which is a Nursing MRT and describes the transition to the role as mastery of behaviors, emotions, signs, and associated resilience to perform new functions, identities, and non-problematic processes that require adopting roles in a preventive or therapeutic way 61.
From the theoretical perspective, situational transitions can be understood as the process of assuming a new role; in other words, ceasing to be spouses or sons/daughters to become FCs of a relative who has suffered a stroke. During this process, caregivers face a series of challenges from the time of diagnosis and during the stroke acute phase to hospital discharge, added to the chronic phase derived from the physical and cognitive sequelae imposed by the disease. Such challenges can ease or hinder progress toward a healthy transition for the caregiver 62.
During the transition to the FC role, its adoption exerts a significant impact on several of the caregivers’ life dimensions (physical, emotional, social, and environmental) and, consequently, it is necessary to implement changes in the relationships, skills and behavioral patterns that allow caregivers to gain self-confidence and develop coping strategies to achieve this healthy transition to their new role 61,62.
Therefore, fostering self-confidence and coping abilities during the transition allows learning and shaping a new attitude and, in the sense of safety, confers meaning from the perspective of the person undergoing the process, as human beings sometimes fail to show themselves confident or prepared to adopt the caregiver role 62,63.
According to Afaf Meleis, transition indicators are response patterns that position a person towards a healthy transition in adopting the role; in other words, they are positive changes in the way in which a person adapts, relates to and copes with their new role. They include developing the necessary skills and competencies to assume the role effectively, as well as developing self-confidence and coping in performing the role responsibilities, in addition to establishing suitable relationships and support networks. These indicators are signs that the person is experiencing an effective and healthy transition in adopting the new role 61.
To guarantee the aforementioned, it is necessary to see the transition as a care opportunity, and Nursing professionals should value the awareness, commitment, changes/differences, time properties, and the critical points of the transition in a transitioning FC to determine the caregiver’s needs. This will allow, from a Nursing therapeutic education, to plan highly effective interventions to ease the transition and expect healthy results; in other words, healthy coping in adopting the role 61-63.
Meleis defines Nursing therapeutic education based on three measures that can be widely applied to therapeutic interventions during transitions, namely: in the first place, appreciating the caregiver’s preparedness from a multidisciplinary approach will allow health professionals and researchers to identify the specific needs during the transition and, in turn, create an individualized profile regarding the client’s preparedness. Secondly, training for the transition is suggested as a Nursing therapeutic measure that includes education as the main modality to create optimum conditions. In the third place, role supplementation was proposed as a Nursing therapeutic measure to shape the role and develop care skills 63,64.
Specifically, Meleis urges health professionals to act as a support source when easing the transition, seeking interventions to solve the needs of the person requiring professional health services 61-63.
Review of the empirical evidence
To explore the current scientific evidence about the transition to the role of caregiver of OAs after stroke, a review of the empirical evidence was conducted in the SciELO, PubMed, EBSCO Host and BVS databases. The articles selected to develop the SST met the following criteria: a) being written in English, Spanish, or Portuguese, b) having been published in the last five years, and c) containing the keywords selected. The health science descriptors used were as follows: Caregiver, Family caregiver, Stroke, Older adult and Aged person; using the AND and OR Boolean operators with the following search strategy: (transición) AND (cuidador familiar) AND (fulget:(“1”) AND mi:(“Cuidadores” OR “Cuidado de Transición” OR “Familia”) AND la:(“en” OR “es”)) AND (mi:[2018 TO 2022]). The search for articles was conducted from September to October 2022. All 692 articles retrieved were sorted by categories and abstraction level; subsequently, they were analyzed in terms of scope, specificity and abstraction, contextual comprehension, and connections with research and practice. Finally, 22 articles discussing topics that reflect the conceptual characteristic to be theorized were extracted. A synthesis of the 22 articles that contain the variables of interest (transition, family caregiver, transitional care, role adoption) regarding the elaboration of this SST proposal is presented below.
Stroke is a common chronic disease that generates high morbidity, disability, and mortality rates, representing a severe threat to the mental health of the survivors and their family members. After the acute phase, most OAs experience various disability degrees such as hemiplegia, numbness, difficulty speaking, and face paralysis, which require care and rehabilitation for more than 18 months. This results in FCs presenting insufficiencies in adopting the caregiver role, which generates emotional distress, depression, and anxiety, exerting a negative impact on their social and economic functions, as well as on their physical health and quality of life 53,54,65,66.
When the family member undergoes a change in their situational role, this transition is experienced as a difficult, complex, and unexpected event that can be either positive or negative based on resilience and coping ability during the stroke acute phase. In this sense, it is necessary to identify the care and self-management needs to develop self-confidence and favor healthy coping 52,65,66.
Self-management implies that the caregiver should be capable of organizing and administering the tasks and demands related to the care to be provided to the OA after a stroke. This includes planning and coordinating medical appointments, medications, rehabilitation therapies, personal care, and monitoring symptoms and changes in the management of the patient, among other aspects. Self-management also implies that the caregivers should be able to take care of themselves, meeting their own physical, emotional, and social needs derived from the demands and wear out inherent to the role, which can lead to burden and exhaustion 44.
FCs’ self-management implies acquiring diverse care-related knowledge and skills regarding the disease, medication, feeding, mobilization and hygiene, risk prevention, rehabilitation, and selfcare to safely apply them both to themselves and the OAs after a stroke in the home environment 67,68. Therefore, offering these resources and adequate support allows for generating and maintaining a proactive and resilient attitude in FCs in the face of the challenges that may arise during the OAs’ chronicity after stroke.
The FC transition should be favored by Nursing therapeutic education as a care instance; therefore, valuing the existing resources allows for easing the transition to devising favorable environments to develop self-confidence, coping, autonomy, and independence for assertive decision-making for the benefit of disabled and dependent OAs after a stroke, thus improving transition and adoption of the role in a healthy way 53,69.
It is to be considered that the core elements of successful Nursing therapeutic education lie in an innovating and multidisciplinary process based on communication between providers and FCs as a way to generate self-confidence and face health-related behaviors to improve role adoption 57,60,69-71.
Therefore, to encourage FCs to develop self-confidence and coping, it is necessary to incorporate specific transition interventions that allow developing care skills and strategies to cultivate confidence, in addition to fostering coping and resilience capabilities in FCs in the face of care-related challenges 54,56. In this sense, it is necessary to assess the caregivers’ needs as home-based care progresses, considering that they also need assistance, care and role supplementation, so that they continue their life plan 57,58,72.
The scientific evidence indicates that, based on Nursing therapeutic education, the multidisciplinary team not only develops care-related knowledge and skills but also generates comprehensive well-being in FCs, which is reflected in self-confidence and coping, autonomy and security in their role as caregivers of OAs after a stroke 21,56,73. In this sense, suitable training of caregivers is a key element for self-management in health services and holistic comprehensive services, provided that it can be considered that FCs undergo an effective transition and a healthy role adoption process 54-56,59,74.
Step D) Theorization of the Situation-Specific Theory
Definition of Concepts
Elaboration of the SST for the transition to the role of caregiver of OAs after a stroke is established from four concepts that are now defined: situational transition to the caregiver role, care-related knowledge and skills, development of FCs’ self-confidence and coping in adopting the role, and, finally, Nursing therapeutic education.
Situational transition to the family caregiver role: It is defined as a stressful period that the person experiences suddenly, given the nature of the stroke, and can be characterized as effective or ineffective. Effective transitions take place when a FC shows preparedness, skill and competence to provide home-based care and, therefore, confer a positive meaning to the role of caregiver. On the other hand, ineffective transitions take place when FCs experience uncertainty, expressed as concern, insecurity, lack of confidence and fear, due to unpreparedness and to lack of skills and competencies to provide home-based care to OAs after a stroke 54,75,76.
Care-related knowledge and skills: Care-related knowledge and skills are determined by the FCs’ self-awareness and by their ability to provide comprehensive care in the following aspects: medication, feeding, nutrition, hygiene, gastrointestinal management, rehabilitation, prevention of injuries, and transfers of OAs after a stroke in the home environment, added to the ability to manage control of chronic-degenerative diseases at health services, in addition to comprehensive and psychological management of the dyad 56,75,77.
Nursing therapeutic education: It is a comprehensive and complementary intervention based on a multidisciplinary approach (Neurology, Nutrition, Rehabilitation, Social Assistance, Psychology). Its objective is to provide theoretical knowledge and generate care-related skills using didactic methods to prepare FCs before, during and after the hospital-home transition 56,73,78.
Development of self-confidence and coping in adopting the caregiver role: It is characterized by the possibility that FCs adopt their role healthily or pathologically. Healthy adoption of the caregiver role is defined by the preparedness, skill and competence to provide home-based care, generating a positive response to the role, its organization and its execution. On the other hand, pathological adoption of the caregiver role is related to ineffective transitions resulting in complications such as physical stress, anxiety, depression, loneliness and impaired quality of life, due to a lack of knowledge, skills and competencies to provide care 79-82, with a possible burden. The integrality of the concepts is shown in Figure 2.
Proposals set forth in the SST: Transition to the Role of Family Caregiver of Older Adults after a Stroke:
The situational transition to the FC role, either effective or ineffective, is directly dependent on the care-related knowledge and skills, on Nursing therapeutic education, and on the development of self-confidence and coping in adopting the caregiver role.
To generate a healthy transition in adopting the caregiver role, Nursing therapeutic education must provide the FC with care- related knowledge and skills focused on the care to be provided to OAs after a stroke.
Nursing therapeutic education exerts a direct influence on the situational transition to the FC role, on the care-related knowledge and skills, and on the development of self-confidence and coping in role adoption.
The development of self-confidence and coping ability for a healthy adoption of the caregiver role is the result of an effective situational transition, influenced by all the knowledge and skills acquired by the FCs through Nursing therapeutic education.
Description of the Theoretical Model
The scheme shown in Figure 2 presents the key concepts that will be used to achieve the “adoption of the caregiver role” specific result. Three sequential phases (from left to right) are described below; they represent the processes as challenges or opportunities for caregivers to assume their role in an effectively.
The first concept addresses the transition to the caregiver role, which marks the beginning of the entry process. This part evidences the opportunity to value such transition, which will allow the consideration of the characteristics that define caregivers concerning their social, political, economic and environmental contexts. In addition, the impact of this transition on the caregiver’s life is analyzed in physical, emotional, social and spiritual terms.
The transition is disaggregated into two conceptual elements. On the one hand, we have effective transitions, which refer to FCs’ preparedness to provide home-based care to people in a chronic situation due to a stroke. In contrast, ineffective transitions carry with them a certain accumulation of negative feelings and uncertainty about the future due to unpreparedness to provide care. They can lead FCs to adopt a pathological role, manifesting unpleasant symptoms such as stress, anxiety and loneliness, which in turn can trigger other psychological symptoms due to burden and impair their quality of life as caregivers.
The second concept refers to care-related knowledge and skills, which are a sequential step toward the objective. It emerges as an opportunity for FCs because it allows raising awareness about the importance of providing good quality and risk-free care, in addition to promoting understanding of the role while performing it. This aspect is fundamental to ease the caregivers’ transition, although its effectiveness depends on the transition indicators, namely: the development of skills, competencies, self-confidence and coping, generated by Nursing therapeutic education to support suitable performance of the role.
Although it is the output or final element, the development of self-confidence and coping in adopting the caregiver role is directly dependent on other key concepts: the caregiver’s situational transition and care-related knowledge and skills, along with Nursing therapeutic education. Healthy adoption of the caregiver role is characterized by self-confidence and effective coping, which are generated through Nursing therapeutic education, as a resource to face role adoption in the home environment. In other words, skills development provides the necessary competence for self-management during the chronic stage of the person cared for. On the other hand, pathological role adoption is distinguished by the presence of physical, psychological and social symptoms related to burden, resulting in impaired quality of life for FCs.
Nursing therapeutic education plays an outstanding role in each of the three aforementioned phases to develop strategies that foster self-confidence, coping skills, knowledge and skills in the caregivers. This leads to raising awareness and understanding about their role, thus ensuring a healthy transition and adoption. It is important to consider that nurses play a fundamental role as main care providers for people undergoing transitions.
Step E) Verification and Validation
Research
As for the current SST, it is precisely in this process that some implications for practice and research are shared with the scientific community. Regarding the practice, it is necessary that Nursing professionals and those from related areas are able to use the SST to validate the content of the theory and sustain the care to be provided 26; it is also necessary that the providers of educational options for multidisciplinary management consider the FCs’ age and schooling level, as the transitions will be eased when the facts and the abstraction and resilience capabilities are better understood while adopting the caregiver role.
In relation to research, the concepts and their inter-relationships can be modified and structured according to the scientific evidence of the concept. For this reason, related areas should apply the SST in intervention, management, and care studies, where a healthy transition to the caregiver role is promoted, as well as Nursing therapeutic education to enhance care-related knowledge and skills in caregivers of people with some chronic condition and to improve coping considering the caregiver role.
Application of empirical indicators
To determine the efficacy of the SST, tests and validation using empirical indicators are required 26, through a pilot study or intervention research with a group of FCs of OAs after a stroke in different areas and environments throughout the country. The current SST presents some specific empirical indicators for each concept established (Table 1).
Table 1 Empirical Indicators to Validate the Situation-Specific Theory
| Concept | Empirical indicator | Variable |
|---|---|---|
| Situational transition to the family caregiver role | Cohen’s Perceived Stress Scale 83. Hospital Anxiety and Depression Scale (HADS) 84. UCLA Loneliness Scale 85 The WHO Quality of Life Questionnaire (WHOQOL-BREF) 86 | Situational transition |
| Care-related knowledge and skills | Scale to assess the caregivers’ care-related skills (CAI) 87. Home-based care competence (CUIDAR) 88 | Care-related skills |
| Adoption of the role of family caregiver of chronic patients (ROL) 69 | ||
| Self-confidence and coping in adopting the caregiver role | Scale to assess the coping and adaptation process (ESCAPAS) 89 | Adoption of the caregiver role |
| Generalized Self-Efficacy Scale (GSES) in non-professional caregivers 90 | ||
| Zarit Caregiver Burden Scale 91 |
Source: Prepared by the authors.
Conclusions
This SST provides a theoretical framework that explains the challenges and requirements during the transition of FCs of OAs after a stroke and why Nursing therapeutic education is the pure essence of Nursing care, that is to say, it provides moments to visibly learn care and self-care in FCs, so that the person develops self-confidence and coping in healthily adopting the caregiver role.
The recommendation is to use this theoretical proposal in the clinical context and Nursing research, both at the undergraduate and graduate levels, with the purpose of turning this SST into a reference framework to develop behavioral interventions in health and educational programs targeted at FCs of OAs after a stroke.
As this is a theoretical proposal based on the integrating approach, some structural and content modifications may be implemented in the future, starting from the fact that the phenomenon is unstable and that, in this sense, this SST can be rejected.
















