Introduction
Over the last few decades, the number of people with chronic and potentially incurable illnesses has increased, resulting in a greater demand for healthcare and a growing need for palliative care 1. Palliative care refers to the provision of care that improves the quality of life of a patient with a potentially incurable illness and of their family, through the prevention and relief of suffering, the early identification of symptoms, and the assessment and treatment of pain and other physical, psychosocial, or spiritual needs 2.
The Political Declaration on Universal Healthcare Coverage 3 reiterates the need to include palliative care in national health policies, advising an approach that integrates coordination at all levels and ensures the overall improvement of healthcare systems. However, there is still a gap in access to palliative care, which is a challenge and a priority for public healthcare worldwide 4.
People in palliative care experience specific health needs that require person-centered care and a joint effort to reduce suffering and improve quality of life 5. Hodiamont et al. 6 emphasize symptom relief, information for autonomous decision-making, and psychosocial and spiritual support to deal with the illness process, considering the participation of caregivers throughout the end-of-life process to be paramount.
When providing care for people with incurable illnesses, humanizing the relationship between the person, their family, and the nurse becomes essential. It is expected that this relationship will result in active and specialized care that promotes suffering relief and the preservation of dignity 7, which is why nurses must integrate the human expression of the disease while respecting g the uniqueness of individuals, their values, beliefs, ideologies, and culture 8. Thus, a gap in the provision of holistic care results in a limitation in the effectiveness of palliative care and adds to suffering in its various dimensions 9.
Comfort is often associated with the relief of suffering and identified as a vital personal need to feel in complete harmony and well-being. Referred to as a transitory and multidimensional experience 10, it is a complex concept 11 recognized as a determinant of the experience lived by the individual and the quality of healthcare 10. However, the scientific evidence is not unanimous in defining the attributes that characterize comfort 12-14, and several studies have focused on the physical dimension to the detriment of the multidimensionality inherent to the concept 15. Nuraini et al. 16 reiterate this stance when they state that, in the process of providing care for people in palliative care, nurses emphasize pain and neglect other areas of comfort, namely psychosocial, cultural, and spiritual needs. Understanding the meaning and significance of comfort as attributed by palliative care patients and their families can be a challenge for nurses 15. The lack of a single, well-established definition, along with the individuality of the meaning attributed by the person in palliative care, hinders the measurement and assessment of comfort needs 15.
Katharine Kolcaba's theory of comfort 17 describes comfort care as improving quality of life and functional status, and it can be a useful theoretical reference for planning nursing care aimed at promoting comfort for people in palliative care 18. It emphasizes the definition of interdisciplinary strategies to promote comfort throughout the illness process, as it focuses on Fawcett's meta-paradigmatic concepts (person, environment, health, nursing) and their impact on the person's comfort 18.
Kolcaba 17 defines comfort as a holistic experience stemming from the response to physical, psychospiritual, sociocultural, and environmental needs to provide relief, ease, and transcendence. Relief refers to the satisfaction of a specific need for comfort. Ease refers to a state of calm and tranquility that allows a person to behave functionally and efficiently. Transcendence refers to the attempt to satisfy the needs that allow for problem-solving, and to plan and control one's destiny. The physical dimension refers to the satisfaction of needs related to bodily sensations and homeostatic mechanisms, and the psychospiritual dimension results from a person's internal awareness of oneself. Kolcaba 17 also addresses sociocultural needs, which encompass interpersonal, family and social relationships, and environmental needs, which represent the external context of the human experience.
When providing care to people in palliative care, nurses must focus on planning and implementing interventions that aim to meet the needs associated with the end of life 15,18. Nursing care for people in palliative care entails the provision of quality care by nurses, to relieve suffering and promote quality of life for people with progressive or life-limiting illnesses and their families, regardless of their state of health, the care required, or the context in which they find themselves 19.
Based on the theory of comfort 17, it is deemed that the systematization of knowledge regarding nursing care in the promotion of comfort for people in palliative care enables the highlighting of the role of nurses in this field of care and can contribute to the definition of strategies that are consistent with the continuous improvement of nursing practices. From the definition of the review question: "Which types of nursing care promote comfort for people in palliative care?", the sub-questions: "What is the influence of nursing care in promoting comfort for people in palliative care?" and "Which population is involved in studies on comfort for people in palliative care?" emerged. In this sense, a scoping literature review was designed to map the available scientific evidence on nursing care that promotes comfort for people in palliative care.
Materials and Methods
A scoping review was conducted based on the Joanna Briggs Institute (JBI) guidelines for this type of literature review 20. The information was organized according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses model - PRISMA 21. To structure the study's written content, the guidelines of the PRISMA for Scoping Reviews checklist were followed -PRISMA-ScR 22. The review protocol was registered on the Open Science Framework (https://doi.org/10.17605/OSF.IO/CN258). As this is a literature review, the study does not require approval by an ethics committee.
Search Strategy
The review question was devised using the "PCC" strategy (population, concept, context), according to the JBI Manual for Evidence Synthesis 20, where the population is people in palliative care; the concepts are comfort and nursing care for people in palliative care, and the context is institutions that provide nursing care for people in palliative care.
The search was conducted in three stages to identify published and unpublished studies. Original studies were included, with publication dates ranging from January 2014 to March 2023, with abstracts and full texts available in open access. Publications in Portuguese, English, and Spanish were included.
In the first step, a limited initial search was performed in the Medline (Medical Literature Analysis and Retrieval System Online/PubMed) and CINAHL (Cumulative Index to Nursing and Allied Health Literature/EBSCOHost) databases to find articles related to the topic being studied and to analyze the text words and indexing terms included in the title and abstract of the articles found. The following strategy was used to identify the articles of interest: "Comfort" [All fields] AND "nurs*" [All fields] AND "palliative care" [All fields].
In the second step, the first author conducted a full search on the Medline Complete, CINAHL Complete, Scopus, and Web of Science search engines to find published studies, and on the Repositório Científico de Acesso Aberto de Portugal (RCAAP) and OpenGrey to find unpublished studies. A combination of descriptors / medical subject headings (MeSH), text words, and indexing terms along with the Boolean operators AND and OR were used. Truncation* was used to enhance the search by creating new variations of the same word. A search syntax adjusted to each database was used (Table 1).
The third step consisted of identifying additional studies from the bibliographic reference lists of the articles included in the scoping review. The reviewer responsible for analyzing article content included in the review proceeded to identify articles of interest in the list of bibliographical references, and these were conditionally included in the list of articles to be analyzed.
Table 1 Search Strategy
Source: Elaborated by the authors.
Inclusion and Exclusion Criteria
All studies that evidenced the influence of nursing care in promoting comfort for palliative care patients were considered. Primary studies were included, with quantitative, qualitative, or mixed-methods methodology, which were conducted in institutions where nursing care is provided to people in palliative care. The research was not limited by the sociodemographic or clinical variables of the sample being studied. Article inclusion was not limited by the type, size, or geographical location of the study setting.
All articles that failed to reflect primary research, such as editorials, concept analysis articles, review articles, letters, theoretical essays, books, or book chapters, were excluded.
Study Selection and Eligibility
The articles obtained from the search were cataloged and imported into the Rayyan Intelligent Systematic Review® software (Cambridge/United States of America, Doha/Qatar), to eliminate duplicate references. To select the relevant studies, two reviewers analyzed the title and abstract independently according to the previously defined eligibility criteria. In the event of discrepancies in title and abstract analysis, a third reviewer was consulted to decide whether to include or exclude the article from the list of articles to be analyzed.
The full texts of the articles to be analyzed were retrieved, and the entire text was studied in detail by two independent reviewers. In the final decision on whether to include or exclude an article, discrepancies were discussed with a third reviewer to reach a consensus. A flow chart adapted from PRISMA-ScR 21 was used to systematize the search results and the study selection process. The articles included in the scoping review were assigned an alphanumeric code (An) which allowed them to be organized in chronological order, from the oldest to the most recent.
Data Extraction and Analysis
All relevant data of interest were extracted and cataloged on a form designed for this purpose. For each study, specific data was considered regarding i) authorship, year, and country of publication; ii) research methodology; iii) sample characteristics; iv) study duration; v) study objective; vi) nursing care that promotes comfort for palliative care patients, and vii) the influence of nursing care in promoting comfort for palliative care patients.
Data extraction and analysis were conducted by two independent reviewers and any discrepancies were settled by a third reviewer. To ensure clarity and consistency in this step, in the first five articles, data extraction and analysis were discussed simultaneously by both reviewers.
The data extracted is presented in diagram and table format, coupled with a narrative summary that highlights the relevant data extracted from the articles. To systematize the data on nursing care that promotes comfort for people in palliative care, the theory of comfort 17 was implemented as a theoretical reference, so the data is g grouped in double-entry tables based on the dimensions and types of comfort defined by the author (relief, ease, and transcendence).
Results
Study Selection
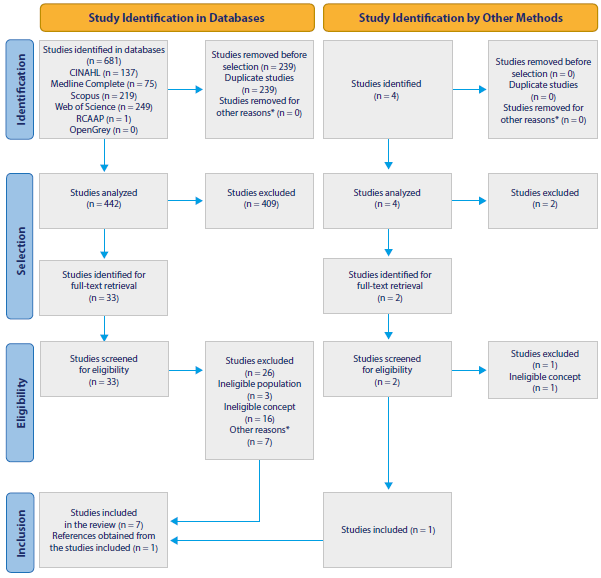
The search strategy retrieved 681 articles, of which 239 were removed for being duplicates. Of the 442 studies selected for title and abstract analysis, 409 were excluded, leading to the retrieval of the full text of 33. Of these, 26 were excluded due to non-compliance with the inclusion criteria: ineligible population (n = 3), ineligible concept (n = 16), or full text unavailable in open access (n = 7), resulting in a total of seven articles included in the scoping review.
Four articles were also found in the bibliographic reference lists of the articles included in the scoping review. Of these, two were selected for full-text retrieval and one was excluded for failing to meet the inclusion criteria in terms of context (Figure 1).
Characteristics of the Study
Qualitative studies (n = 6) represent most of the studies identified, with only two adopting a quantitative approach 23,24. As far as the sample is concerned, one study was conducted on patients with stage II or higher cancer 24, one on professionals who are part of a multi-professional team 25, and the others on nurses 23,26-30. Three studies conducted in Brazil 25-27 and three in Indonesia 24,28,29 were also identified. Only one study was conducted in Europe 23.
Table 2, which summarizes the characteristics of the studies included in the scoping review, shows that the data collection time ranged from 4 days 27 to 6 months 23, with three studies not reporting this data 24,28,30.
Table 2 Main Characteristics of the Studies
| Study ID Country/ Language | Type of Study | Sample | Study Duration | Objective |
|---|---|---|---|---|
| A126 Brazil/English | Qualitative study | 4 nurses and 6 nursing technicians with more than one year of clinical practice in intensive care units | 3 months | To understand the meaning of nursing care for a comfortable death from the perspective of an intensive care nursing team |
| A227 Brazil/ Portuguese | Qualitative exploratory study | 13 nurses from the nursing team of an intensive care unit | 4 days | To describe the nursing team's perception of palliative care and pain management |
| A328 Indonesia/ English | Qualitative study | 8 nurses with clinical practice experience in oncology | Not stated | To describe nurses' perspective on the comfort of patients in palliative care |
| A4 23Czech Republic/ English | Descriptive, cross-sectional, quantitative study | 201 nurses with at least one year of clinical practice in departments where they frequently provide care to end-of-life patients or those with a potentially incurable chronic illness | 6 months | To determine the frequency of Dying Care Nursing Intervention Classification activities performed by nurses on end-of-life patients |
| A5 29 Indonesia/ English | Phenomenological, descriptive, qualitative study | 10 nurses with certified training in palliative care | 3 months | To explore and understand the meaning assigned by nurses to comfort children at the end of life |
| A624 Indonesia/ English | Cross-sectional, quantitative study | 308 patients with stage II or higher neoplasms and no central nervous system metastization | Not stated | To develop a theoretical model that statistically fits the data and can examine the factors that affect the comfort of people with cancer with physical and emotional mediators |
| A725 Brazil/ Portuguese | Exploratory, descriptive, qualitative study | 50 professionals (13 nurses, 13 medical doctors, 9 physiotherapists, 9 nursing technicians, 3 nutritionists, 2 social workers, 1 psychologist) | 6 months | To analyze the multiprofessional team's perception of comfort at the end of life in intensive care units |
| A830 Peru/Spanish | Qualitative study | 6 nurses and 6 family caregivers of people with terminal cancer | Not stated | To describe the friendship, comfort measures, and support provided by spiritual care to people with terminal cancer, according to the perception of nurses and family caregivers in a hospital in Chiclayo, Peru |
Source: Elaborated by the authors.
Characteristics of the Participants
Two of the studies identified did not detail the sample characteristics 27,29. A total of 612 individuals participated, of which 255 were nurses and 15 were nursing technicians. In the studies by Silva et al. 26, Nuraini et al. 28, Kisvetrová et al. 23, Pires et al. 25 and Ayasta et al. 30, most participants were female. In the study with patients 24, the prevailing diagnosis was stage III breast cancer (n = 139) and most of them (n = 251) received care on an outpatient basis. Three studies were conducted in intensive care units 25-27, in which 30 nurses and 15 nursing technicians participated. One study was conducted with nurses and family caregivers 30 and another with nurses providing care to children at the end of life 29.
Nursing Care that Promotes Comfort
In the study by Pires et al. 25, which was conducted with a sample consisting of multidisciplinary professionals, only the data that emerged from the answers provided by nurses was considered to meet the objective of the literature review. The data extracted reflects nursing care that promotes comfort in people in palliative care, using the theory of comfort 17 as a theoretical reference.
In the data analysis, nursing care aimed at promoting relief, ease, and transcendence was identified in the physical, psychospiritual, environmental, and sociocultural dimensions (Table 3). In the physical dimension, the management of symptoms such as pain, nausea, and respiratory discomfort is the focus of attention when defining nursing care. The most frequently mentioned interventions are administering analgesia 23,25-29, monitoring pain 23,28-30, and positioning the patient 23,26,27,30. Respecting dietary preferences 23,25,30, reducing respiratory discomfort by administering sedatives and oxygen 26,28,30, performing relaxation techniques 23,26,29 and hygiene care 23,26,30 were identified as nursing care that provides relief and allows patients in palliative care to find a state of calm and tranquility.
Table 3 Nursing Care to Promote Comfort for People in Palliative Care
Source: Elaborated by the authors.
In terms of meeting psychospiritual needs, nursing care focused on supporting the family in the grieving process 23,26,27,29 and on reducing anxiety and fear by implementing pharmacological measures 23,27,28 and promoting dialogue 23,25,26. Care such as religious support 24,25,28 and help in understanding the uncertainty of the diagnosis 23,25,26 were also identified in this dimension.
Regarding the environmental dimension, nursing care that promotes comfort in people in palliative care consists of reducing noise 27,28,30, providing a calm and familiar environment 23,25,26,28, and making organizational rules more flexible to allow the presence of family members or significant others 23,25,26,28,30 and the use of personal objects 23,25,26,28.
Concerning the satisfaction of sociocultural needs, nursing care reflects concern not only for interpersonal, family, and social relationships but also for rituals and religious practices. Ayasta et al. 30, Kisvetrová et al. 23, Nuraini et al. 28, Pires et al. 25, and Silva et al. 26 highlighted the relevance of the presence of family members and significant others and encouraging family participation in care and decision-making. Other studies 23,24,26-28 emphasize communication, namely through conveying adequate information regarding diagnosis, prognosis, treatment, and the patient's path.
The Influence of Nursing Care in Comfort Promotion
In the study by Silva et al. 26, conducted with nurses and nursing technicians, the promotion of comfort expresses care for a good death, which includes the relief of physical discomfort, social and emotional support, and body to maintain the health of the person in palliative care. Comfort results from therapeutic interventions that reconcile rationality and sensitivity, with respect for dignity emerging from the relationships between professionals, the person, and their family 26.
Data analysis indicates the importance of the role of nurses in end-of-life care, as they are the healthcare professionals who are closest to the person in palliative care and who know their uniqueness 26,27. Defining and implementing nursing care aimed at promoting comfort results in minimizing suffering, improving quality of life, and managing pain 24,27-30.
Discussion
Providing palliative care for people can be a challenge. Nurses are expected to adopt a holistic approach and provide humanized care that meets the uniqueness of the person and their family, who have their wishes and specific emotional, spiritual, and social needs 8. Comfort is associated with the relief of suffering and is regarded as a complex, dynamic, subjective, and positive experience 17 that integrates experiences and concepts such as quality of life, hope, control, and decision-making 31. In the relationship with the person in palliative care and their family, it is important to establish an empathetic relationship based on the principles of Humanitude. In palliative care, the focus is on the person and their family, and the multidisciplinary team has a key role in meeting their needs throughout the health-disease process. Due to their proximity to the person and their family, nurses are the healthcare professionals expected to be most willing to act efficiently in all dimensions of comfort.
The literature review highlights nursing care that promotes comfort for people in palliative care, reflecting the role of nurses in the care process and the multidimensionality inherent to comfort. Based on the 5 analysis of the studies found, nursing care focused on the management = and control of physical symptoms 23,25-30, psycho-spiritual support 23-29, environmental management 23,25-30 and family support 23-30 emerged. The definition and implementation of multidimensional plans will contribute to an effective response, not only focusing on the management of physical symptoms, but also integrating the person's spirituality, emotions, and relationships with their significant others. Tools such as Humanitude and an empathetic relationship are crucial to the success of the therapeutic relationship between the nurse and the person in palliative care and their family. Communication is particularly important throughout the care process.
In addition to the progression of the disease in palliative care patients, the worsening or onset of physical symptoms such as pain, respiratory discomfort, delirium, altered state of consciousness, and digestive or cardiovascular symptoms often lead to hospitalization 32, which is why it is important to define a nursing care plan centered on the person and their family.
Nurses' perception of pain in palliative care patients is a determining factor in their quality of life and can be reflected in the | morbidity related to their health condition 33. Pain and the fear of pain are reasons for concern expressed by palliative care patients and their families, sometimes coupled with the feeling of total pain, reflected in physical, social, emotional, and spiritual suffering. In the scenario of chronic and potentially incurable diseases, physical pain management emerges from the definition of pharmacological and non-pharmacological interventions, where communication between nurses and patients assumes an epicentric position 7,33. In their literature reviews, Silva et al. 26, Aquino et al. 27, Nuraini et al. 28, Kisvetrová et al. 23, Suryani et al. 29, Pires et al. 25, and Ayasta et al. 30 highlighted pain monitoring and analgesia administration as nursing care that promotes comfort. However, other types of nursing care such as minimizing invasive procedures 25,26, positioning patients 23,26,27,30, and using relaxation techniques 23,26,29 were identified as contributing factors to pain management.
In palliative care, spirituality is relevant to relieving the patient's physical and psychospiritual suffering, as well as that of the family and healthcare professionals 34. Psycho-spiritual suffering consists of feelings of anxiety and fear, whereas respect for religious and cultural beliefs 23-25,28, the promotion of dialogue 23,25,26, and effective communication with the patient and their family to help them understand the uncertainty of the diagnosis 23,24,26-28 are nursing care measures that relieve suffering and promote a feeling of tranquility and transcendence.
In this literature review, support for the family during the illness process and bereavement 23,26,27,29 was identified as nursing care that facilitates the satisfaction of needs that allows patients to feel capable of solving problems as well as planning and controlling their destiny. In palliative care, family caregivers transcend relationships of bloodline, including friends or other significant people with emotional or social ties 35. Family caregivers often experience feelings of physical and psychological overload and, simultaneously, need to readjust their personal and professional lives to the new role of being a caregiver. In this sense, a holistic understanding of the needs of the person in palliative care and their family becomes the foundation for defining a nursing care plan centered on promoting comfort. Becqué et al. 36 reiterate that identifying the needs of family caregivers is essential for providing personalized care and support and that nursing care has a positive influence on the outcomes of family caregivers.
Healthcare organizations must implement an organizational culture that includes strategies that allow healthcare teams to engage in self-care multidimensionally to be able to provide quality care for others. Demystifying palliative care among all healthcare professionals is still a challenge, which is why there is an urgent need for action in this field of professional training. It is therefore essential to continue the efforts to provide specific training in the palliative care field so that health teams are strengthened in terms of its dimension, but also in terms of the skills and behaviors aimed at providing care for people in palliative care.
Study Limitations
In this literature review, a systematized research strategy was used which allows for the clear translation of the research method and study replication. However, the interpretative synthesis inherent to the content analysis of the studies identified results in a certain level of subjectivity that can reduce transparency.
When interpreting the data from this review, some limitations should be considered. The research strategy focused on nursing care that promotes comfort for people in palliative care. However, comfort, as a multidimensional concept, is sensitive to the intervention of other healthcare professionals, and nursing care includes prescription-dependent interventions, which may result in nursing care that, despite contributing to the promotion of comfort, was not identified in the studies.
The time limit set, as well as studies available only in English, Portuguese, and Spanish, may result in a bias in the interpretation and scope of the results. Most studies were conducted with small sample sizes. The prevalence of qualitative methodology may justify this fact, and some authors have referred to saturation as a criterion for defining sample size.
As this is a scoping review, the quality of the studies was not analyzed, but the inclusion of all the articles identified demonstrates the state of the art in this field of research.
Conclusions
Defining comfort assessment tools can help to relieve the suffering of people in palliative care, as it allows the causes of discomfort to be identified and a nursing care plan to be devised that is targeted at the patient's needs. The provision of person- and family-centered care is vital in promoting comfort, and the individualization of care and the response to specific needs can result in relief, ease, and transcendence.
The theory of comfort 17 was presented as a useful theoretical reference in the systematization of nursing care to promote comfort for people in palliative care. It was noted that this type of care focuses on the person and their family, and it integrates the various dimensions of the concept. The potential for engagement and articulation between pharmacological and non-pharmacological interventions in controlling and managing symptoms and strengthening the person's quality of life was identified.
A more comprehensive literature review, of the systematic review type, and conducting studies that establish the causal relationship between the nurse's intervention and comfort for people in palliative care are suggested.