Remark
| 1) Why was this study conducted? |
| To determine the effects of central intermittent theta-burst stimulation and repetitive peripheral magnetic stimulation on upper limb function. |
| 2) What were the most relevant results of the study? |
| Combining the two treatment methods can improve patients' motor function and daily living abilities but cannot improve muscle tone. |
| 3) What do these results contribute? |
| To find a better treatment plan for the rehabilitation of upper limb function. |
Introduction
Upper limb hemiplegic paralysis caused by stroke is a common problem in the clinic. Repeated transcranial magnetic stimulation is a non-invasive brain stimulation technology that can continuously stimulate the premotor cortex of the cerebral cortex, increase its excitability, and help improve the recovery of limb function and limb spasms. Currently, it is used as an effective intervention method to restore the motor nerve function of the upper limb 1,2. The most commonly used region of repeated transcranial magnetic stimulation to improve upper limb function is the primary motor cortex (M1 region) of the brain 3, and studies have demonstrated that stimulating this region can significantly improve upper limb function 4. Repeated transcranial magnetic stimulation can regulate the imbalance of activity between the motor cortex of the hemispheres caused by brain damage. Thus, balancing the excitability of the dual hemispheres of the cortex promotes functional recovery 5.
Intermittent theta burst stimulation (iTBS) is a new type of repeated transcranial magnetic stimulation treatment modality. It mimics the pulse release frequency of the human hippocampus 6, improves the excitability of the cerebral cortex and induces long-term potentiation of cortical excitability. At the cellular level, iTBS-induced long-term potentiation amplifies the effects of exercise training 7. iTBS can change the neuroplasticity of the brain and facilitate the recovery of motor function 8. Compared with repeated transcranial magnetic stimulation, short-term stimulation can cause changes in cortical excitability, enhance cortical plasticity, and bring it closer to the physiological state of neural activity. It has a strong effect and short duration and can achieve a good curative effect in a short period. iTBS has become a commonly used transcranial magnetic stimulation treatment in clinical practice. Repetitive peripheral magnetic stimulation (rPMS) is a non-invasive treatment method that is administered with high intensity outside the brain. In rPMS, coils are placed on the trunk and limb muscles. A magnetic field passes through the skin and generates an action potential, which excites the nerve muscle. rPMS can improve limb function, relieve spasticity 9, and improve motor function 10,11.
Intermittent theta burst stimulation and rPMS use magnetic stimulation to stimulate different sites separately. Although many studies have confirmed their effectiveness in treating upper limb function. There is a lack of research on rPMS combined with iTBS in treating upper limb dysfunction after stroke. This study aimed to test whether rPMS and central iTBS are more beneficial for the recovery of upper limb function in stroke patients than either stimulation modality alone.
Materials and Methods
Participants
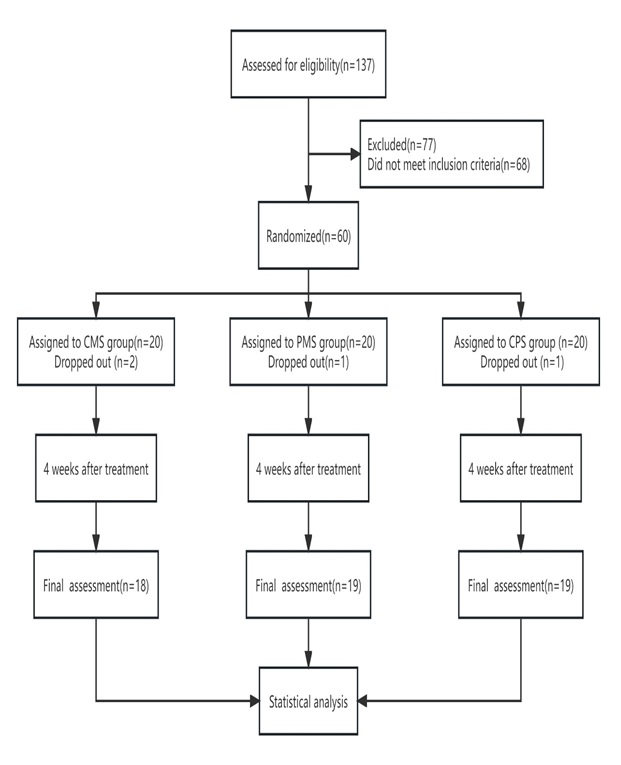
This study was a randomized, parallel-design, double-masked controlled trial (Clinicaltrials.gov identifier : ChiCTR2300068838). The local ethical committee approved the study (No. 2022-475). Sixty stroke patients with hemiplegia were hospitalized in our hospital from January 2022 to December 2022 (Figure 1). Random Allocation Software (RAS) was used to randomly divide all participants into the following three groups according to a 1:1:1 ratio: central magnetic stimulation (CMS) group, peripheral magnetic stimulation (PMS) group and CPS group (Intermittent theta-burst stimulation combined with repetitive peripheral magnetic stimulation). Only the magnetic stimulation equipment operator was aware of the group assignments; the stroke patients, rehabilitation therapists, and rehabilitation assessors were unaware of the group assignments. All participants signed informed consent forms. The inclusion criteria were as follows: 1) First ischemic stroke, confirmed by neuroimaging (CT or MRI) 12; 2) Unilateral cerebral apoplexy upper limb motor dysfunction; 3) An onset time of 15 days to 3 months and a stable condition; 4) 45-75 years old; and 5) Sufficient cognition to understand the purpose and follow the instructions of the study Mini-Mental State Examination (MMSE) score ≥24). The exclusion criteria were as follows: 1) An unstable condition, including severe heart, lung, or renal insufficiency; 2) A history of epilepsy or a family history of epilepsy; 3) Previous motor dysfunction caused by other diseases; 4) Heart pacemakers and metal implants in the brain; and 5) Fear of treatment or intolerance.
Procedures
All patients were given routine medical therapy and conventional rehabilitation therapy. Conventional rehabilitation therapy includes exercise therapy, physical therapy, occupational therapy, speech therapy and so on. The duration of each session was 40 minutes, and the sessions occurred once a day for five days a week for four weeks.
Patients in the CMS group received iTBS stimulation of the affected head area. This study used CCY-I TMS l (Wuhan Eruid Medical Equipment New Technology Co., Ltd.) and a figure-eight coil. . Using a built-in device, and the iTBS stimulation protocol was designed to stimulate the upper limbs. The coil was fixed with a stent to the functional representative area of the upper limb of the M1 region of the affected side of the patient's brain. The iTBS stimulation protocol consisted of 600 pulses with a frequency of 50 Hz within the plexus, 5 Hz between the plexus, 2 s stimulation and 8 s intervals. The stimulation duration was 3 min 20 s, and the intensity was 30% of the resting motor threshold. The resting motor threshold was determined by observing the maximum flexion of the contralateral index finger achieved in more than 5 out of 10 single-pulse stimuli. Then, patients in the CMS group received peripheral false stimulation, with the stimulation site and time being the same as those in the PMS group described below, but the sound was played without generating stimulation. The treatment was given once a day for five days a week over four weeks.
The PMS group first received central false stimulation. The stimulation site and time were the same as those in the CMS group mentioned above; however, a sound was played, while stimulation was not applied. After central false stimulation, peripheral magnetic stimulation was performed. The stimulation site of the PMS group was the Erb point of the affected limb, which was 2-3 cm above the clavicle about the width of a transverse finger behind the sternocleidomastoid muscle. The branches of the brachial plexus were concentrated and superficial, the best site for stimulating the brachial plexus. The subject was placed supine with the limb in the good limb position. The center point of the coil was placed as close to the Erb point as possible, and the stimulation frequency was 10 Hz, with 3 s of each stimulus, 8 s of rest, and a total of 1200 pulses. Each intervention lasted 7 min 20 seconds, and the stimulation intensity was 30% of the resting motor threshold. The treatment was given once a day for five days a week over four weeks.
In the CPS group, the above central stimulation was performed first, followed by peripheral stimulation, and the treatment parameters were the same as above.
Outcome measures
Functional assessments were performed by the same trained rehabilitation therapist before and after four weeks of treatment to evaluate clinical efficacy in all three groups.
The Fugl-Meyer assessment (FMA): The FMA was used to evaluate the improvement in upper limb function before and after treatment. The FMA consists of 33 items, including the function of the affected shoulder and elbow, wrist joint flexor and extensor cooperative movement, wrist joint stability and other functions. The maximum score of each item is two points, with a full score of 66. The greater the total score, the better the patient's upper limb motor ability.
Modified Barthel Index (MBI): Activity of daily living (ADL) was assessed by the MBI, including 11 items, such as washing and going up and down stairs, with a total score of 100. The higher the score, the better the patient's activity level and the less dependent they are on others.
Action Research Arm Test (ARAT): The ARAT was used to evaluate upper limb movement, including grasping, gripping, pinching and gross movement, with a total score of 57. The higher the total score, the better the fine motor function.
Modified Ashworth Scale (MAS): The MAS is divided into six levels to evaluate the muscle tone of the hemiplegic side. The higher the grade is, the higher the tension. Grades 0, I, I+, II, III, and IV are recorded as 0, 1, 1.5, 2, 3 and 4 points, respectively.
Data analysis
The data analysis was performed using SPSS version 24.0. The Shapiro-Wilk test was used to confirm the normal distribution of all outcome variables. The chi-square test and one-way analysis of variance (ANOVA) were used to compare the baseline characteristics of the three groups. The paired sample t-test was used for comparisons within the three groups, and the differences between the three groups before treatment, after treatment, and before and after treatment were analyzed using one-way ANOVA, and further pairwise comparisons were performed using the least significant difference (LSD) test. A value of P < 0.05 was considered statistically significant.
Results
A total of 137 patients were enrolled, and 77 were excluded; of the latter, 68 were excluded because they did not meet the exclusion criteria, and another nine withdrew from the trial because they were unwilling to continue treatment. Finally, 60 patients were enrolled in the study. During the treatment, two patients dropped out in the CMS group, 1 in the PMS group and 1 in the CPS group due to the patient's unwillingness to continue the training and the patient's request for discharge. The general characteristics of the patients in the three groups are shown in Table 1. Statistical analysis showed that there was no significant difference between the three groups (p >0.05), indicating comparability (Table 1).
Table 1 General characteristics of the subjects
| Group | n | Gender(n) | Age(year) | Duration(day) | Type(n | Hemiplegic side(n) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Infarction | Hemorrhage | Left | Right | |||||
| central magnetic stimulation | 18 | 11 | 7 | 59.78±5.33 | 10.50±1.65 | 10 | 8 | 8 | 10 | |
| repetitive peripheral magnetic stimulation | 19 | 12 | 7 | 59.37±4.57 | 11.37±1.38 | 9 | 10 | 10 | 9 | |
| CPS | 19 | 11 | 8 | 60.42±4.62 | 10.68±1.49 | 10 | 9 | 9 | 10 | |
| p value | 0.378 | 0.797 | 0.190 | 0.673 | 0.687 | |||||
Before treatment, there were no significant differences in the FMA score, MBI, ARAT score or MAS score among the three groups (p >0.05). After treatment, the FMA score, MBI and ARAT score in the three groups were significantly increased compared with those before treatment (p <0.05). After treatment, the FMA, ARAT and MBI in the CPS group were significantly different from those in the CMS and PMS groups (p <0.05), while there was no significant difference in the MAS between the three groups after treatment and before treatment (p >0.05) (Table 2).
Table 2 Clinical testing results (x ±s)
| CMS group(n=18) | PMS group(n=19) | CPS group(n=19) | p value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Decrease | Pre | Post | Decrease | Pre | Post | Decrease | ||
| FMA | 22.78±5.58 | 34.67±9.30 | 11.89±3.72 | 21.53±4.79 | 31.05±5.52 | 9.52±0.73* | 23.32±6.63 | 39.37±5.86 | 16.06±0.69* # | 0.002** |
| MBI | 39.72±6.06 | 63.33±5.42 | 23.61±0.66 | 38.16±5.06 | 61.32±4.96 | 23.16±0.19* | 38.16±4.48 | 67.11±4.81 | 28.95±0.34* # | 0.002** |
| ARAT | 26.17±1.62 | 35.06±2.10 | 8.89±0.48 | 26.74±2.00 | 35.63±2.43 | 8.89±0.43* | 27.00±2.71 | 37.75±3.26 | 10.75±0.55* # | 0.012** |
| MAS | 0.81±0.64 | 0.92±0.67 | 0.11±0.03 | 0.95±0.57 | 1.13±0.64 | 0.18±0.07 | 1.13±0.62 | 1.16±0.55 | 0.04±0.07 | 0.753 |
*Compared with the CMS group, p <0.05
#Compared with the PMS group, p <0.05
**The comparison of Decrease among three groups, p <0.05
Discussion
In our study, we found that the motor function scores of all groups after treatment were significantly increased compared with those before treatment, while the MAS score showed no significant change.
TBS is an extension of traditional repeated transcranial magnetic stimulation therapy. The treatment regimen for TBS simulates the coupling of theta oscillation and gamma rhythm within the cortex 13. TBS can be divided into intermittent TBS (iTBS) and continuous TBS (cTBS). iTBS can increase the excitability of the motor cortex, while cTBS has the opposite effect. iTBS is more effective than cTBS in recovering upper limb function after stroke 14. iTBS has been widely used to improve limb function, speech, cognition and swallowing function in patients after stroke 15-17. It can achieve high-frequency stimulation in the short term and cause cortical excitatory changes 18. It has the characteristics of a short stimulation time, low intensity and high frequency. iTBS stimulation of the affected M1 can increase the excitability of the affected cortical motor area in early stroke patients, with a significant increase in cortical excitability lasting for 20-30 minutes. The M1 area of the primary motor cortex is thought to be the main source of inputs to descending spinal cord neurons that ultimately connect with the surrounding muscles. The M1 area is also considered a key region for the execution and planning of hand and upper limb movements and plays a key role in cortical reorganization during the recovery of upper limb motor function. After the stroke, the cortical excitability of the bilateral cerebral hemispheres changes, and the inhibition between the hemispheres is unbalanced. The existing balance between the two cerebral hemispheres is broken, and the inhibitory effect of the affected hemisphere on the healthy hemisphere is weakened 19. Like repeated transcranial magnetic stimulation, iTBS can alleviate this imbalance 20, increasing the excitability of the M1 area on the affected side 21. It can balance the excitation of the bilateral M1 area and promote the recovery of motor function. In 26 stroke patients with hand movement disorders who were treated with iTBS in the M1 area, it was found that patients in the M1 stimulation group had significantly enhanced grip strength recovery and increased motor network connectivity levels but not in the parieto-occipital vertex (control-stimulation group) 22.
The enhancement effect of iTBS was similar to that of high-frequency repeated transcranial magnetic stimulation. In a study of 42 chronic stroke patients, iTBS was initiated before robot-assisted training. It was found that iTBS may facilitate poststroke motor learning by enhancing the permissiveness of the ipsilesional sensorimotor area to therapeutic sensory modalities 23. iTBS treatment can improve the motor function of stroke patients, especially fine motor function 24. In 12 patients with subacute stroke, stimulation at 1,200 pulses/session in the M1 region was also tolerated, and the patients showed improvement in motor function 25. The physiological mechanism by which iTBS can improve motor function is thought to possibly reduce motor dysfunction caused by brain injury in early stroke by regulating microglia 26. Studies have also found that iTBS can produce similar changes to the long-term potentiation and long-term depression through the regulation of GABA receptors 27. Therefore, iTBS may be an effective way to improve upper limb function after a stroke. The present study showed that the FMA score, MBI, and ARAT scores of patients in the CMS group were significantly higher than those before treatment, confirming that iTBS improved upper limb motor function in stroke patients.
After the stroke, the structural lesions of the brain make the neural network disordered, and repeated transcranial magnetic stimulation can improve the imbalance of the damaged brain. Currently, two kinds of magnetic stimulation treatment methods exist: central stimulation (repeated transcranial magnetic stimulation) and peripheral stimulation (rPMS). Central stimulation, especially in the M1 region, can improve patients' upper limb function. For some patients with traumatic brain injury and cranioplasty, the treatment of rPMS can help them find an alternative way to replace central stimulation. Patients can still benefit from rPMS treatment. rPMS can promote brain plasticity by magnetic stimulation of muscles and peripheral nerves to improve the motor function of patients. rPMS stimulates motor axons to induce action potentials that trigger muscle contraction. rPMS also stimulates the central nervous system by acting on muscles to induce proprioceptive input. Studies have found that rPMS can increase cortical motor center activity and induce neural network reorganization 28. Electrical stimulation commonly used in clinical practice, such as TENS, often causes different degrees of pain symptoms in patients. However, magnetic stimulation can reduce afferent sensory nerves 29 and stimulate deeper nerve structures to reduce pain. rPMS also plays a role in improving spasticity 30. In terms of improving motor function, although some studies have shown that rPMS can improve limb motor function, favorable evidence is still lacking 31. The present study showed that the FMA score, MBI, and ARAT scores of patients in the PMS group were significantly higher than those before treatment, suggesting that rPMS can improve motor function in stroke patients. In a study of healthy subjects, rPMS enhanced wrist extension movements by increasing cortical excitability 32, explaining why rPMS can improve motor function in stroke patients.
The Kruskal‒Wallis test was used to compare groups. The PMS group improved the FMA score, MBI and ARAT score. However, the overall improvement was not as high as that in the CMS group. The reason may be that PMS directly stimulates the sensorimotor afferent nerve fibers to transmit nerve impulses forward and backward to the primary sensorimotor cortex and ultimately promotes the reorganization of brain networks, while iTBS directly stimulates the neurons in the surrounding area of the lesion, improves the survival rate of neurons and increases the excitability of the affected hemisphere and synaptic plasticity in brain regions outside the lesion area. iTBS can improve limb function directly through central regulation, so its effect is more pronounced. Our study found that the CPS group had significant improvements in motor function, activities of daily living and complex movement of the hand compared with the groups administered either of the two treatments alone (p <0.05). In the CPS group, not only was iTBS directly applied to the corresponding functional areas of the brain to increase the excitability of the affected hemisphere, but rPMS was also applied to the Erb point of the affected upper limb to stimulate the contraction of the affected upper limb muscles and activate the self-sensory axis, which carries mechanical sensory information and is the principal axis of muscles and deep connective tissue sensors. The afferent information is transmitted through sensory pathways via thalamocortical projections and then to the primary sensory cortex, changing the discharge of interneurons in the cortex, inducing long-term potentiation of motor cortex synapses through the structural and functional connections between the primary sensory cortex and M1, driving the reorganization of M1 and increasing the excitability of the affected hemisphere; these changes ultimately increase the excitability of the affected hemisphere. Therefore, CPS was more effective in improving upper limb function than CMS and PMS. In the present study, there was no significant alleviation of spasticity and no significant change in MAS scores in the three groups, which may have been due to the lack of sensitivity of the MAS for spasticity and the lack of detailed grading.
A limitation of this study is that we had a small sample size and did not follow up with the patients. Therefore, future studies with larger numbers of patients are necessary.
Conclusion
Our results show that both central iTBS and rPMS alone were able to improve patients' motor function and daily living abilities but not muscle tone. Central iTBS combined with rPMS can improve upper extremity function and daily living ability in patients with subacute stroke. However, the improvement in muscle tone was not obvious.