Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
International Journal of Psychological Research
Print version ISSN 2011-2084
int.j.psychol.res. vol.9 no.1 Medellín Jan./June 2016
Metereological conditions and Psychiatric Emergency Visits in Messina, Italy
Condiciones Meteorológicas y visitas a Emergencias Psiquiátricas en Messina Italia
Salvatore Settineria, Massimo Mucciardib, Valentina Leonardic, Stefan Schlesingere, Mara Gioffrè Florioe, Fausto Famàd, Maria R. Anna Muscatelloa, Carmela Mentoa,*
a Department of Biomedical and Dental Sciences and Morphofunctional Imaging, University of Messina, Italy
b Department of Economics, University of Messina, Italy.
c MD, Specialist in Psychiatry, University of Messina, Italy.
d Emergency Department, University Hospital of Messina, Messina, Italy
e Department of Human Pathology, University Hospital of Messina, Italy.
Corresponding author: Carmela Mento, Dipartimento di Neoroscienze, Université degli Studi di Messina, Messina, Italia. Email address: cmento@unime.it.
Article history: Received: 21-08-2015 Revised: 25-11-2015 Accepted: 10-12-2015
ABSTRACT
Objective: The aim of this study is to examine the association between psychiatric disease, climatic and seasonal factors in patients recorded to the Emergency Unit, in Messina Hospital (Italy).
Method: A total of 6565 psychiatric patients were recorded to the Emergency Unit in Messina from January 2005 and December 2010. Each psychiatric visit in emergency, was categorized by date of appearance and admitting diagnosis according to diagnostic categories: Anxiety, Mood Disorders and Psychosis. Local weather data were obtained from the Metereological Instituted "Aereonautica Militare" station in Messina, Sicily, In addition, to gathering data on the state of the sky, temperature, atmosphericpressure with the normalized value at sea level, relative humidity, rainfall, wind direction and speed, the station is connected to a buoy located on the eastern sector of Tyrrhenian Sea. Results: In anxiety disorders we have found relevant results comparison between winter and spring (p=.007) and spring and fall (p=.001). In affective disorders the differences occur in relation to winter and fall (p=.002), spring and fall (p=001), spring and summer (p=002). The psychotic disorder presents significant differences between summer and fall (p=.001) and spring and fall (p=.002).
Conclusions: We can observe a similarity of affective disorders, i.e. anxiety and mood disorders compared to psychosis, which have different influences and probably according to dissimilar etiopathogenetic ways. In our research, the distribution of anxiety disorders is higher than depressive disorders in terms of delivering emergency room visits. The major differences occur comparing spring and fall, the seasons when all pathological classes have significant differences. It follows that the most abrupt climate change, typical of these seasons, as a whole, cause psychopathological emergencies. The study is important for planning a more effective assistance for patients needing psychiatric support.
Key words: weather, psychopathology, psychiatric emergency visits.
RESUMEN
Objetivo: El objetivo de este estudio fue examinar la asociación entre las enfermedades psiquiátricas y los factores climáticos y estacionales, en los pacientes registrados en la Unidad de Emergencia, en el Hospital de Messina (Italia). Método: 6565 pacientes psiquiátricos se registraron a la Unidad de Emergencia en Messina entre enero de 2005 y diciembre de 2010. Cada visita psiquiátrica en urgencias fue clasificada por fecha de aparición y diagnóstico de admisión de acuerdo con las categorías diagnósticas: ansiedad, trastornos del humor y psicosis. Datos meteorológicos locales se obtuvieron de la Institución Metereológica "Aereonautica Militare" estación en Messina, Sicilia. Además, para la recopilación de datos sobre el estado del cielo, temperatura, presión atmosférica con el valor normalizado a nivel del mar, la humedad relativa, la precipitación, la dirección del viento y la velocidad, la estación está conectada a una boya situada en el sector oriental del mar Tirreno.
Resultados: En los trastornos de ansiedad se encontraron resultados relevantes en comparación con el invierno y la primavera (p = 0,007) y primavera y otoño (p = 0,001). En los trastornos afectivos se produjeron diferencias en relación con el invierno y el otoño (p = 0,002), primavera y otoño (p = 001), primavera y verano (p = 002). El trastorno psicótico presenta diferencias significativas entre verano y otoño (p = 0,001) y en primavera y otoño (p = 0,002).
Conclusiones: Podemos observar una similitud de los trastornos afectivos; es decir, los trastornos de ansiedad y del estado de ánimo en comparación con la psicosis, los cuales tienen diferentes influencias y probablemente formas etiopatogénicas diferentes. En nuestra investigación, la distribución de los trastornos de ansiedad fue más alta que los trastornos depresivos en términos de la entrada de visitas a la sala de emergencia. Las principales diferencias se produjeron comparando la primavera y el otoño, las estaciones del año cuando todas las clases patológicas tienen diferencias significativas. De ello se deduce que el cambio climático más abrupto, típico de estas estaciones, en su conjunto provoca situaciones de emergencia psicopatológicas. El estudio es importante para la planificación de una asistencia más eficaz para los pacientes que necesitan ayuda psiquiátrica.
Palabras clave: clima, psicopatología, visitas a emergencias psiquiátricas.
1. INTRODUCTION
Complex psychopatological phenomena are determined an interaction of individual and environmental factors (Mann et al, 1999). Seasonality seems to be associated with increased suicide counts and depressive symptoms, in the general population (Page et al, 2007; Preti 1997; Huibers et al, 2010). Among the latter, meteorological conditions, which have been shown to have an impact on the human beings (Sulman, 1984). The literature suggests a relationship between weather conditions and affective disorders, in example mood disorders (Molin et al, 1999; Lee et al, 2007), anxiety disorders (Bulbena et al, 2005), psychosis and impulsiveness (Volpe et al, 2008; Shory et al, 2003).
Seasonal and climate factors may represent the determinants of health care utilization and psychiatric hospitalization costs. In an attempt to elucidate the chronopsy and meteotropism in psychiatric psychopathology have examined the chronograms of, and the biometeorological relationships to bed occupancy of a psychiatric ward during three consecutive years (1987-1989) (Maes et al, 1993). The number of psychiatric beds occupied during the study period exhibited a significant seasonal variation suggesting that short-term fluctuations in atmospheric activity may dictate some of the periodicities in psychiatric psychopathology. A study showed a relationship between seasonal visits in the summer and fall and the number of of patients with mood disorders, neurotic stress-related and somatoform disorders recorded (Singh et al, 2007). A review about seasonal affective disorder (SAD), described, thoroughly byboth retrospective and prospective studies, the actuality of seasonal variation in mood and that, in the general population, depressive symptoms peak in winter, and the most extreme form of this disposition, SAD, appears to be a relatively common disorder (Magnusson, 2000).
Metereological factors such as temperature, sunshine and rainfall seem good candidates. In facts, it is a common and well-spread belief that people become "depressed" when the weather is bad, and feel happy when the sun is shining (Watson, 2000). Climatic variables have been found to modulate known biological correlates of affect such as plasma tryptophan and serotonin availability (Maes et al, 1995; Sarrias et al, 1989; Radua et al., 2010). Panic anxiety was found to be more frequent during days with the warm western-origin poniente wind and during fall, and less frequent during rainfall (Bulbena et al, 2007). Episodes of panic were more common with the ponente wind (hot wind) twice less often rainfall, and one and a half times more common in fall than in other seasons (Bulbena et al, 2005). Vulnerability to seasonal changes seems to be a separate dimension of bipolar disorder (Volpe et al, 2008; Volpe et al, 2010). Studies of psychiatric and community samples provide robust evidence that the occurrence of psychosis, aggression and suicide (Shiloh et al, 2005; Kaplan et al, 1996; Lee et al, 2006; Deisenhammer et al, 2003).
Recently, it was revealed that higher illuminance of daytime, greater fluctuation in sleep time, and lower central serotonergic function significantly and independently predicted hyperthymic tendency (Hoaki et al, 2011). Terao & Hoaki (2011) investigated the association between illuminance of daytime and Hamilton depression rating scale (HAM-D) scores and that between illuminance of daytime and Young mania rating scale (YMRS) scores. The findings revealed the significantly negative association between illuminance of daytime and HAM-D scores indicating that light can ameliorate low mood in healthy people. Infact, when handled properly, controlled light exposure can be used to treat some mood and sleep disorders and this is consistent with several researches that have shown a potential antidepressant effect of infrared irradiation (Dumont & Beaulieu 2007; Tsai et al, 2007). Sunshine exposure has been a central focus in mood disorders in response to seasonal changes, and is thought to possibly result in the alteration of monoamine neurotransmitter activity between seasons, both serotonin and dopamin levels observed in patients affected by SAD (Koskela et al, 2008; Hsiang -Yi et al, 2001). To this effect, data have shown consistently over the last 50 years that patients suffering from depression experience a wide range of circadian rhythm disturbances (Kennaway, 2010; Erren et al, 2011). Interestingly, there were numerous reports of decreased melatonin production in depression which may explain the use of melatonin, as well as synthetic melatonin agonist (MT1/MT2 receptor), to improve sleep disturbances in the context of mood disorders (McIntyre et al, 1989; Nair et al, 1984, Gorwood, 2010). The literature suggests that there is a surprisingly direct relationship between weather conditions and a variety of disordered behaviors (Christensen et al, 2008; Yacherson et al, 2011; North et al, 1998). Moreover, meteorological conditions have been linked psychiatric admission rates (Briere & Downes, 1983; Daniels et al, 2000).
Although are several researches on the relationship between climate and psychiatric disorders, few studies have focused on the relationship between climatic factors and emergency psychopathology, also in Sicily.
The aim of this study is to examine the association of psychiatric disorders with the weather in the emergency visits. Particularly, we propose to study the seasonal variations in the number of patients' visits with psychiatric diagnosis and to evaluate the factors contributing to increase of observation of psychiatric cases at Emergency, according climatic conditions (i.e. humidity, wind) of our area (Messina).
2. METHOD
A 6565 patients were recorded to the Emergency Unit of the Policlinic "G. Martino" in Messina (Italy), in the emergency access of psychiatric disease, during a period from January 2005 to December 2010, for a total 2.157 days. Each emergency visit, was categorized by date of appearance and admitting diagnosis according to DSM -IV TR into main diagnostic categories: Anxiety (including panic disorder, general anxiety, stress-related disorders), Mood Disorders (depressive and bipolar disorders, somatization and conversion disorders, drug/alcohol abuse) and Psychosis (Schizophrenia and other psychotic disorders, psychomotor agitation). Local weather data were obtained from the Metereological Instituted "Aereonautica Militare" station in Messina, Sicily, at 51 meters at sea level and the geographical coordinates 38° 12'N 15° 33'E. In addition to gathering data on the state of the sky (cloudiness), temperature, atmosphericpressure with the normalized value at sea level, relative humidity, rainfall, wind direction and speed, the station is connected to a buoy located on the eastern sector of Tyrrhenian Sea, through which you can observe the state of the sea, the height of wave, the direction of the wave. In particular, meteorological data for each of the corresponding days consisted of maximum daily temperature (tmax l0), minimum daily temperature (tmin l0), maximum (rhmx l0) and minimum (rhmn l0) relative humidity, precipitation 00-12 hours (pr1_l0) and precipitation 12-24 hours (pr 2_l0), wind speed (wind l0), direction of wind (dir l0) and sunshine (sun l0). Moreover for each weather variable delays have been considered up to a maximum of seven days (see the symbols 1_2_3_4_5_6_7 in the tables).
2.1 Statistics
We have adopted three approaches to measure the effects of weather variables on Psychiatric Emergency Visits (PEV) for each season. The Mann-Whitney U-test were used to test whether daily means for PEV classified for mental disease (Anxiety, Mood and Psychosis), differ across the seasons. The non-parametric Spearman's correlation coefficient was applied to identify possible correlations between PEV (classified for mental disease) and meteorological variables. Finally, in order to further examine this relationship, a multiple logistic regression were applied to model days with/without PEV for each class of mental disease controlling for season. The climate variables were selected using the stepwise forward conditional regression model with p = 0.05 for inclusion and p= 0.10 for exclusion.
The corresponding odds ratio (OR), with 95% confidence intervals (CI), were obtained for every selected variable. Significance is reached when the 95% confidence intervals do not include 1. All analyses were performed using SPSS (13.0) and Excel 2003.
3. RESULTS
In our study, between pathological disease and seasons different averages are observed (table 1 and 2). Table 1 summarizes the data on emergency department visits for the three pathological disease (anxiety disorders, mood disorders and psychosis) from 2005 to 2010 tor a total of 2157 days. For anxiety disorders we have found relevant results in comparison between winter and spring (p =. 007) and between spring and fall (p =. 001). In affective disorders, the differences occur in the relationship between winter and fall (p =. 002), spring and fall (p =. 001) and between spring and summer (p =. 002). The psychotic disorder presents significant differences when comparing the summer and fall (p =. 001) and between spring and fall (p =. 002). In the fall, for Anxiety, has been observed a correlation between weather and the presentation to the emergency room, particularly the role of maximum and minimum temperature and wind. The minimum temperature has significant relationships both on the day of the visit (r = 0.1947, Sig. 0.001) than in the 3 days before to the visit (r = 0.1826, Sig.0, 001, r = 0.1769, Sig. 0.001; r = 0.1689, Sig. 0.001). A similar pattern occurs for the maximum temperature on the day of the visit (r = 0.1511, Sig. 0.001) and 3 earlier days (r = 0.1621, Sig. 0.001, r = 0.1611, Sig. 0.001; 0.1462, Sig. 0.001). Other significant correlations occur in the days prior to the visit, but less high. Wind direction plays a special role in the two days before the visit (r = 0.1150, Sig. 0.001, r = 0.1243, Sig. 0.001). The humidity has a reverse direction to anxiety. The maximum relative humidity decrease from 7th up to 5th day before the visit would increase the presence of the phenomenon of anxiety (r = -0.2179, Sig. 0.001, r = -0.1911, Sig. 0.001, r = - 0.1118, Sig. 0.001). In spring there are no clear directions between climatic parameters and the phenomenon of anxiety. In summer a forward correlation between the maximum and minimum temperature as it has for the fall (Sig. 0.001). A similar phenomenon occurs for the minimum relative humidity in the opposite direction the second day before the visit to emergency room (r = - 0.1170 Sig.0, 001). Also the precipitation that correlates inversely with anxiety the fourth day before the visit (r = - 0.1331, Sig.0, 001). In winter we observe all the phenomena occur in a reverse direction (Sig. 0.001) compared to the phenomenon of anxiety. In particular, the minimum temperature at the third and fourth days before the visit (r = - 0.1180 Sig. 0.001, r = - 0.1590 Sig. 0.001) and the maximum temperature the previous day (r = - 0.1189 Sig. 0.001) until the fourth day before the visit (r =- 0.1122, r = -0.1180, r = - 0.1608, Sig. 0.001). Even the maximum and minimum relative humidity have significant negative correlations with the winter.
In the fall affective disorders are related to the minimum and maximum and temperature on the same day of observation (respectively r = 0.1379, Sig. 0.001 and r= 0.1369, Sig. 0.001), and the minimum temperature during the five earlier days. As anxiety disorders, there is an inverse correlation with maximum relative humidity that's important the seventh day before the visit (r = - 0.1166 Sig. 0.006). In the spring we find no correlation.
In winter there is an inverse correlation between climatic parameters and affective disorder, with particular reference to relative humidity maximum, minimum and maximum temperature from the third to seventh day prior to observation in the emergency room.
In summer the maximum humidity has a significant correlation with regard to the same day and the day before the visit (respectively r = 0.1264, Sig. = 0.003 and r = 0.1620, Sig. 0.001).
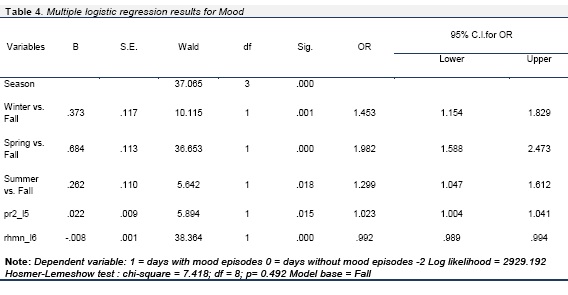
In fall the Psychosis there are no significant correlation. Spring has just reverse correlations for the parameter of the wind on the sixth day before the presentation to the emergency room (r = - 0.1495, Sig. 0.001). The summer has a direct relationship between the maximum relative humidity and psychotic episodes (r = 0.1243, Sig. 0.004) and inverse with the minimum temperature on the fourth and fifth day before the visit (r = -0.1490, Sig. 0.001 and r = - 0.1163, Sig.0.007). The winter correlates inversely with maximum relative humidity (r = - 0.1343, Sig. 0.001).The logistic regression model (Table 3,4,5) for the three pathological classes (anxiety, mood and psychosis) takes the fall as a baseline and allows to highlight predictive aspects of emergency visits as a function of changes in weather and seasonal factors. With reference to anxiety, a higher incidence of emergency room visits is evident in the spring (OR=2.041) followed by winter (OR=1.834).
The maximum temperature and wind three days before play an important role. Conversely, the minimum relativity humidity seven days before decreases the probability having anxiety symptoms. About the mood, spring (OR=1.982) is the most representative season followed by winter (OR=1.453) and summer (OR=1.299). The precipitation (12-24 hours) five days before increases (slightly) the probability that mood disorders occur. In contrast, the minimum relative humidity decreases (fairly) the probability of occurrence of affective disorders in the next six days. For psychosis, in the summer there is more probability of occurrence of acute episodes (OR=2.032) and, only secondarily, in the spring (OR=1.337). The difference between the several conditions and seasons allows us to observe unique behavior in the comparison between winter and spring, not unique in the comparison between winter and summer and differences in individual diseases between winter and fall, spring and summer for the mood disorders, between summer and fall for psychosis, and between spring and fall for all psychopathological spectrum. So, the major differences occur comparing spring and fall, the seasons when all pathological classes have significant differences. It follows that the most abrupt climate change, typical of these seasons, as a whole, cause psychopathological emergencies.
In reference to the values weather we do not observe variables that increase the probability of so clear onset of the disease. Especially temperature on the seventh day before and wind on the sixth day before decreases the probability of having the presentation to the emergency room.
4. DISCUSSIONS
In our research, clinical data are related to meteorological those in a population that comes from a urban district Messina. The distribution of anxiety disorders is higher than depressive disorders in terms of delivering emergency room visits. In relation to season, the spring is most representative in which there is the absolute increase of all admissions, either because of individual diseases. This one in agreement with most studies in the literature (De Graaf et al, 2005; Howart & Hoffman 1984; Bulbena et al, 2005).
According climatic factors, there are significant variables and less significant others. The maximum and minimum temperature influence the emergency department presentations on different days by the climatic variation leads us to presume that the influence of climate element can not be immediate but may have latency periods, as in the case of anxiety disorder. The episodes of anxiety present, therefore, a perceptual sensitivity to changes in weather. Since the individual climatic factors do not have a uniform pattern (eg, temperature and humidity), it is possible that the same factors act independently of one another. There are not many studies in the literature on the relationship between meteorological factors and anxiety, but the recent findings on the relationship between anxiety and mood could justify our reflections, rather well documented for affective disorders, eg. seasonal affective disorder (Oyane et al, 2008). More generally, the anxiety is associated with depression when the seasonality takes over.
In our study, many epidemiological studies confirm this result, but other ones have also highlighted generalized anxiety associated with markers of seasonal variation; also known as the season has an influence even in the autonomic nervous system, as demonstrated by recent studies on sleep, hypertension and metabolic syndrome (Ohtani et al, 2006; Magnusson, 1996; Oyane et al, 2010). Anxiety and depression are associated with a biological substrate in which represent different aspect of the same problem (Damasio, 1994). In general behavioural changes were noted in the personality and more specifically about the presence of syndromes associated with a spectrum of seasonality (Madden Pamela et al, 1996).
For mood disorders, climate variables have significant correlations that are comparable to those in the anxious condition except for the summer, in which the two conditions correlate differently, in particular anxiety in direct proportion with the maximum and minimum temperature and depression with maximum relative humidity. In fact, in summer the heat is perceived subjectively higher than the actual value of the temperature due to humidity. Also in depressive disorders implicated emotions are sadness and irritability that a humid weather usually favors (Winkler et al, 2006). Volpe et al investigated the existence of a seasonal distribution of three dimensions of mania, psychosis, aggression and suicidality, during psychiatric hospitalizations, in a Brazilian sample (Volpe et al, 2008). Psychosis was positively correlated with hours of sunshine of index month and with increasing hours of sunshine; but negatively correlated with relative humidity of index month and with difference from previous to index month.
5. CONCLUSION
In our study, the climatic phenomena that affect psychosis does not have a univocal reading. The number of observations is lower than the whole sample and the diagnosis of psychosis includes a range of psychopathological symptoms that is not homogeneous and this makes more difficult a plausible interpretation of the data. Results from multiple logistic regression model are displayed for each class of mental disease. As we said, our goal is to understand if the psychiatric emergencies are associated with meteorological variables controlling for the seasons.
For anxiety the seasonality (the difference between spring and fall, winter and fall) and climatic factors, above all the maximum temperature and wind direction three days before are predictive of recurrence of the disorder. A similar prediction can be made for mood disorders, for which the season (particularly the difference between spring and fall) and the precipitation (12-24h) five days before can predict the emergence of this pathology. For psychosis comparison between summer and fall has predictive value, while the minimum temperature and wind direction are climatic factors that decrease the probability of acute episodes of psychosis present to the emergency room.
Moreover, climatic factors variety exist both in relation to the their own value that the disease in question; critically, we can observe a certain similarity between anxiety disorders and mood disorders compared to psychosis, which have rather different influences and probably according to dissimilar etiopathogenetic ways. In spite of the studies that find no correlation (Huibers et al, 2010), we believe that these are possible only if the phenomenon is observed in a period not only concurrent with the psychiatric disorder onset, but also in the days preceding; it is possible that all the biological and neurotransmitter changes need different times than the disease, eg. psychosis involving different sectors of the mind.
A limit of this study is that the diagnostic categories are heterogeneous and this is inherent in the problem of emergencies that do not always allow the identification of the nosographic diagnosis with a consequent remarkable dispersion. In contrast, we would underline the importance of having created a method of organizing data upgradeable (databank of 2157 days) which allowed us to merge weather data with medical data daily, through a large sample.
This implementation will allow Hospital of Messina to have a system for forecasting of emergency psychopathology as a function of weather data. The study should this information can be helpful to physicians in planning a more assistance for patients needing psychiatric support.
6. ACKNOWLEDGEMENTS
We are grateful to Prof. Mucciardi for the Statistical analysis.
7. REFERENCES
Briere J, Downes A. Summer in the City: Urban Weather Conditions and Psychiatric Emergency-Room Visits. Journal of Abnormal Psychology 1983; 92, 1: 77-80. [ Links ]
Bulbena A, Pailhez G, Aceña R, Cunillera J, Rius A, Garcia-Ribera C, Gutiérrez J, Rojo C.Panic anxiety, under the weather? International Journal of Biometeorology. 2005; 49 (4): 238-243. [ Links ]
Bulbena A, Sperry L, Pailhez G, Cunillera J. Panic attacks: Weather and season sensitivity? Psychiatry and Clinical Neurosciences. 2007; 61: 129. [ Links ]
Christensen EM, Larsen JK, Gjerris A, Peacock L, Jacobi M, Hassenbalch E. Climatic factors and bipolar affective disorder. Nordic Journal of Psychiatry 2008; 62(1): 55-8. [ Links ]
Damasio AR. Descartes error: emotion, reason and the human brain. New York, Grosset/Putnam. 1994. [ Links ]
Daniels BA, Kirkby KC, Mitchell P, Hay D, Mowry B. Seasonal variation in hospital admission for bipolar disorder, depression and schizophrenia in Tasmania. Acta Psychiatrica Scandinavica 2000; 102,1: 38-43. [ Links ]
De Graaf R, Van Dorsselaer S, Ten Have M, Schoemaker C, Vollenberg WAM. Seasonal variation in mental disorders in the general population of a country with a maritime climate: findings from the Netherlands mental health survey and incidence study. American Journal of Epidemiology 2005; 162, 7: 654-661. [ Links ]
Deisenhammer EA, Kemmler G, Parson P. Association of meterological factors with suicide. Acta Psychiatrica Scandinavica 2003;108: 455-459. [ Links ]
Dumont M, Beaulieu C. Light exposure in the natural environment: Relevance to mood and sleep disorders. Sleep Medicine. 2007; 8: 557-565. [ Links ]
Erren TC, Nise MS, Meyer-Rochow VB. Latitude, light, clocks and mood. Psychopharmacology 2011; 216:147-148. [ Links ]
Gorwood P. Restoring circadian rhytms: a new way to successfully manage depression. Journal of Psychopharmacology. 2010; 24(8) Supplement 2: 15-19. [ Links ]
Hoaki N, Terao T, Wang Y, Goto S, Tsuchiyama K, Iwata N. Biological aspect of hyperthymic temperament: light, sleep, and serotonin. Psychopharmacology. 2011; 213 (2-3):633-8. [ Links ]
Howarth E, Hoffman MS. A multidimensional approach to the relationship between mood and weather. British Journal of Psychology 1984; 75: 15-23. [ Links ]
Hsiang-Yi T, Kao Chin C, Yen Kuang Y, et al. Sunshine-exposure variation of human striatal dopamine D2/D3 receptor availability in healthy volunteers. Progress in Neuro-Psychopharmacology & Biological Psychiatry 2011; 35: 107-110. [ Links ]
Huibers MJ, De Graag LE, Peeters FP, A. Does the weather make us sad? Meteorological determinants of mood and depression in the general population Psychiatry Research 2010; 180 (2): 143-146. [ Links ]
Kaplan Z, Schild K, Levine J. Violence in hospitalized psychiatric patients: diurnal and seasonal patterns. Psychiatry Research 1996; 60: 199-204. [ Links ]
Kennaway DJ. Clock genes at the haeart of depression. Journal of Psychopharmacology 2010; 24(8) Supplement 2: 5-14. [ Links ]
Koskela A, Kauppinen T, Keski-Rahkonen A, Sihvola E, Kaprio J, Rissanen A, et al. Brain serotonin transporter binding of [123I] ADAM: within-subject variation between summer and winter data. Chronobiology International 2008; 25: 657-65. [ Links ]
Lee HC, Lin HC, Tsai SY, Li CY, Chen CC, Huang CC.Suicide rates and the association with climate: a population-based study. Journal of Affective Disorders 2006; 92: 221-226. [ Links ]
Lee HC, Tsai SY, Lin HC. Seasonal variations in bipolar disorder admissions and the association with climate: A population-based study. Journal of Affective Disorders 2007; 97: 61-69. [ Links ]
Madden Pamela AF, Andrew Heath C, Norman Rosenthal E, Nicolas Martin G. Seasonal changes in Mood and Behavior. The role of genetic factors. Archives of General Psychiatry 1996; 53: 1. [ Links ]
Maes M, De Meyer F, Peeters D, Meltzer H, Schotte C, Scharpe S, et al. The periodicities in and biometeorological relationships with bed occupancy of an acute psychiatric ward in Antwerp, Belgium. International Journal of Biometeorology 1993; 37(2): 78-82. [ Links ]
Maes M, Scharpé S, Verkerk R, D'Hondt P, Peeters D, Cosyns P, et al. Seasonal variation in plasma tryptophan availability in healthy volunteers. Relationship to violent suicide occurrence. Archives of General Psychiatry 1995; 52: 937-946. [ Links ]
Magnusson A. An overview of epidemiological studies on seasonal affective disorder. Acta Psychiatrica Scandinavica 2000; 101: 176-184. [ Links ]
Magnusson A. Validation of the Seasonal Pattern Assessment Questionnaire (SPAQ). Journal of Affective Disorders. 1996; 40: 121-129. [ Links ]
Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. American Journal of Psychiatry 1999; 156:181-189. [ Links ]
McIntyre IM, Judd FK, Marriott PM, Burrows GD, Norman TR. Plasma Melatonin Levels in Affective States. International Journal of Clinical Pharmacology Research 1989; 9: 159-164. [ Links ]
Molin J, Mellerup E, Bolwig T, Scheike T, Dam H. The influence of climate on development of winter depression. Journal of Affective Disorders 1999; 37:151 - 155. [ Links ]
Nair NP, Hariharasubramanian N, Pilapil C. Circadian rhythm of plasma melatonin in endogenous depression. Progress in Neuro-Psychopharmacology & Biological Psychiatry 1984; 8(4-6): 715-8. [ Links ]
North CS, Pollio DE, Thompson SJ, Spitznagel EL, Smith EM. The association of psychiatric diagnosis with weather conditions in a large urban homeless sample. Social Psychiatry & Psychiatric Epidemiology. 1998 May;33(5):206-10. [ Links ]
Ohtani T, Hisanobu K, Tareshi U, Ken I, Nobumasa K, Tsukasa S. Sensitivity to seasonal changes in panic disorder patients. Psychiatry and Clinical Neurosciences 2006; 60: 379-383. [ Links ]
Ojane NM, Ursin R, Pallesen S, Kolsen F, Bjorvatin B. Increased Health risk in subjects with high self-reported seasonality. Plos One 2010, 5, 3: e9498. [ Links ]
Oyane NMF, Byelland I, Pallesen S, Holsten F, Bjorvantn B. Seasonality is associated with anxiety and depression: The Hordaland health study. Journal of Affective disorders. 2008; 105:147-155. [ Links ]
Page LA, Hajat S, Kovats RS. Relationship between daily suicide counts and temperature in England and Wales. British Journal of Psychiatry 2007;19:106-112. [ Links ]
Preti A. The influence od seasonal change on suicidal behaviour in Italy. Journal of Affective Disorders. 1997; 44:123-130. [ Links ]
Radua J, Pertusa A, Cardoner N. Climatic relationship with specific clinical subtypes of depression. Psychiatry Research. 2010; 175: 217-220. [ Links ]
Sarrias MJ, Artigas F, Martinez E, Gelpi E. Seasonal changes of plasma serotonin and related parameters: correlation with environmental measures. Biological Psychiatry 1989; 26: -. [ Links ]
Schory TJ, Piecznski N, Nair S, El-Mallakh RS. Barometric pressure, emergencypsychiatric visits and violent acts. Canadian Journal of Psychiatry. 2003; 48: 624-7. [ Links ]
Shiloh R, Shapira A, Potcher O, Hermesh H, Popper M, Weizman A. Effects of climate on admission rates of shicophrenia patients to psychiatric hospital. European Psychiatry 2005; 20: 61-64. [ Links ]
Singh GP, Chavan BS, Arun P, Sidana A. Seasonal pattern of psychiatry service utilization in a tertiary care hospital. Indian Journal Psychiatry 2007; 49: 91-5. [ Links ]
Sulman FG. The impact of weather on human health. Review on Environmental Health 1984; 4: 83-119. [ Links ]
Terao T, Hoaki N. Light can ameliorate low mood in healthy people. Psychopharmacology. 2011; 213 (4):831. [ Links ]
Tsai JF, Hsiao S, Wang SY. Infrared irradiation has potential antidepressant effect. Progress in Neuro-Psychopharmacology & Biological Psychiatry 2007; 31: 1397-1400. [ Links ]
Volpe FM, Da Silva EM, Dos Santos TN, De Freitas DEG. Further evidence of seasonality of mania in the tropics suicidality. Journal of Affective Disorders. 2010; 124: 178-182. [ Links ]
Volpe FM, Tavares A, Del Porto JA. Seasonality of three dimensions of mania: Psychosis, aggression and suicidality. Journal of Affective Disorders 2008; 108: 95-100. [ Links ]
Watson D. Mood and temperament. The Guilford Press. New York 2000. [ Links ]
Winkler D, Pjrek E, Konstantinidis A, Praschak-Ieder N, Willeit M, Stastny J, et al. Anger attacks in seasonal affective disorder. The international journal of neuropsychopharmacology 2006; 9(2): 215-9. [ Links ]
Yackerson NS, Zilberman A, Todder D, Kaplan Z. The influence of several changes in atmospheric states over semi-arid areas on the incidence of mental health disorders. International Journal of Biometeorology 2011; 55(3): 403-10. [ Links ]