Introduction
Obesity, defined as excess body fat, with a body mass index (BMI) above 30 kg/m2, has become a public health problem, affecting more than 650 million adults worldwide in 20161,2.
In the urological field, obesity has been associated with an increased risk of urolithiasis, infertility, obstruc-tive urinary symptoms, urinary incontinence, genital prolapse, erectile dysfunction, and chronic kidney disease3,4. In recent years, interest in the impact that obesity has on sexual function and fertility has increased5, although it has been seen that abnormalities in sexual reproduction and function are often ignored or not studied in comparison with cardiovascular comorbidities6. Surgical treatment of obesity has been associated with improvement in reproductive hormones, seminal parameters, and symptoms associated with hypogonadism.
The objective of our work is to carry out a systematic review of the effects of bariatric surgery on fertility in patients with obesity.
Materials and methods
Study design
The systematic review was carried out using the PICO method to answer the research question: What are the effects on fertility in obese patients undergoing bariatric surgery?
Search strategies
Included articles were identified in the literature by searching the following databases: PubMed, Lilacs, Scopus, and Cochrane. Only articles were chosen between the years 2012 and 2021.
The search strategy was carried out with the following controlled terms such as and free text: "Fertility" OR "Fecundability" OR "Fecundity" OR "Differential Fertility" OR "Fertility Determinants" OR "Subfecundity" OR "Fertility Preferences" OR "Below Replacement Fertility" OR "Marital Fertility" OR "Natural Fertility" OR "World Fertility Survey" OR "Fertility Incentives" AND "Bariatric Surgery" OR "Metabolic Surgery" OR "Bariatric Surgical Procedures" OR "Stomach Stapling" AND "Obesity" The search syntax was carried out with Boolean operators, which were adapted to the data-bases used.
Eligibility criteria
As inclusion criteria, articles that discussed the fertility outcomes of patients undergoing bariatric surgery were considered; publications with their own data analyzing the effects of bariatric surgery on fertility; that the language of publication was English or Spanish, and that they were published between the years 2012 and 2021. Articles inaccessible to full text were excluded from the study; as well as those that only had theoretical data; and those that did not have results.
Study selection
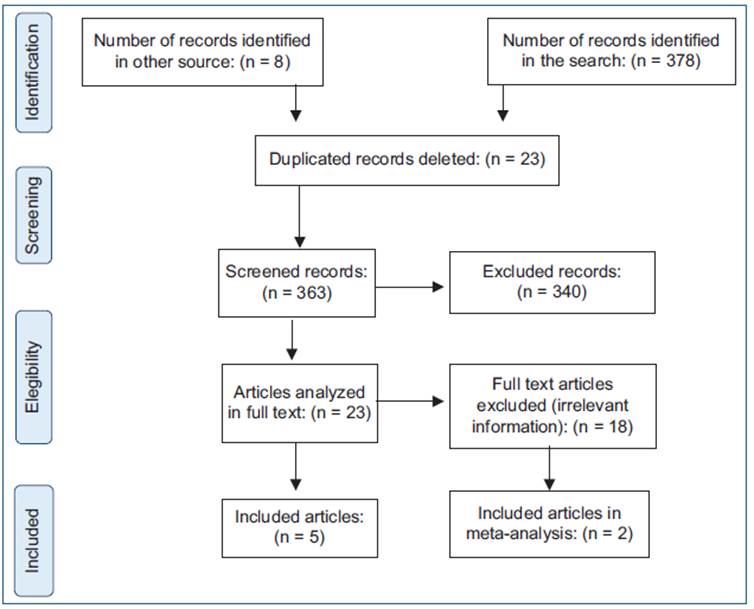
The search yielded a total of 384 results. The titles and abstracts of the articles were reviewed by one of the authors. Articles that were duplicated and those that did not meet the eligibility criteria were eliminated. Finally, the remaining articles and their references were thoroughly manually reviewed in search of additional articles that could be included in this review, including five publications.
Data extraction
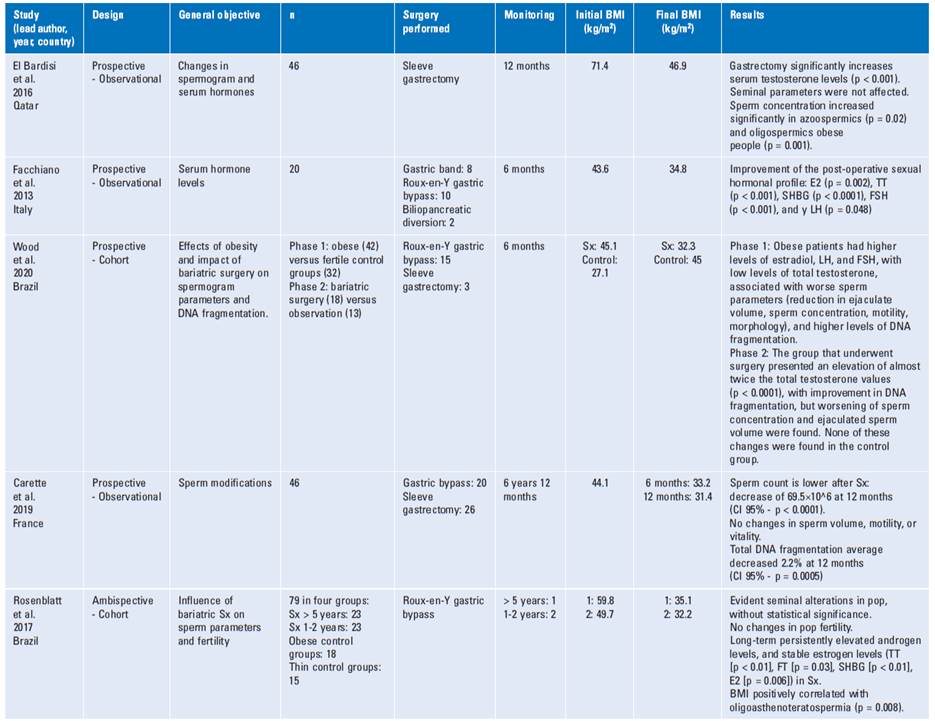
For each study, data were extracted and recorded in a spreadsheet. The main author of each study was registered with the year of publication, country and affiliation of the authors, design, general objective, number of subjects studied, surgery performed, evaluation methods, evaluation times, BMI at the beginning and at the end, change in BMI/weight, and results/ conclusions in terms of fertility.
Quality assessment
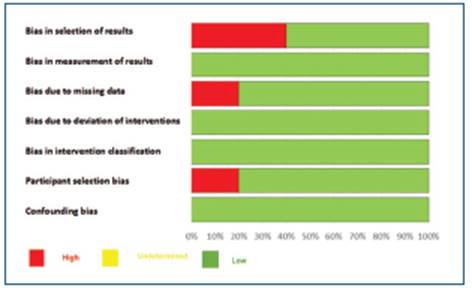
To assess the methodological quality of the included studies, the Cochrane-ROBINS-I tool for non-randomized studies7 was used, which includes the type of biases shown in table 1 and figure 1.
Studies are not excluded based on these results and were classified as high, indeterminate, or low risk. Publication bias was assessed by constructing the funnel plot.
Results
Five articles were analyzed for a total population of 279 patients, whose general objective was to evaluate the impact of bariatric surgery on sperm parameters and/or hormonal parameters. Figure 2 shows the flowchart that summarizes the search and selection process of the articles.
Characteristics of the studies
Table 2 summarizes the characteristics of the included studies and table 1 summarizes the evaluation of the articles with the ROBINS-I tool. The biases ratio in the studies is found in figure 1.
Total testosterone and free testosterone levels
Regarding total testosterone levels, all the articles measured the values before and after the procedure, finding in all a statistically significant improvement in post-operative levels in patients undergoing bariatric surgery. In the study by Bardisi et al., this increase was equivalent in the three groups, both the initial azoospermia and the oligospermia and patients with previous normal seminal analysis7, although in some studies, no correlation was found between this increase and the improvement in seminal parameters8, regarding this increase compared to the age of the patient, no differences were found in the increase of these values between patients younger than 35 years (p < 0.028, n: 7) and older than 35 years (p < 0.972 n: 13)9. In the studies in which these values were compared with control groups, this difference was even more marked in the patients who underwent the surgical procedure, with an average of 537 ng/dL in those operated versus 371.4 ng/dL in those who were not (p < 0.01)10, and 604 ng/dL (p < 0.0001) versus 200.5 ng/dL (p = 0.46), respectively11.
Free testosterone was calculated in two of the five articles: Facchiano et al. showed an increase from 0.204 nM to 0.251 nM, without achieving a statistically significant difference (p = 0.1)9, while in the control groups, these values were lower (303.9) compared with the operated patients (365) p < 0.0310.
Estradiol levels
Regarding estradiol levels, these presented a slight decrease in their values in the post-operative period, from 135 pg/mL to 130 pg/mL (7), 35-33 pg/mL (8), 149.5-112 pmol/L (p = 0.002)9, where only one article showed a slight increase, being 33.3-32 pg/mL not sta-tistically significant (p = 0.68)11. In relation to the studies of operated patients versus control groups, levels of 39 pg/mL were found in control groups versus 35 pg/ mL in those treated (p < 0.01)10.
LH and FS H levels
Consistent with the secondary hypogonadism that obese patients present, normal or low levels of LH andbFSH are present both before and after the surgical procedure, findings evidenced in all the studies analyzed in this review.
Sex hormone binding globulin (SHBG) levels
SHBG levels were measured in three of the five studies analyzed, evidencing as expected considering the pathophysiology of hypogonadism secondary to obesity given by the decrease in the levels of this globulin, the patients showed a marked and statistically significant increase of its values, from 19 to 39 nM (p < 0.0001)9, and lower levels in the placebo group (27.7 nM) versus those undergoing bariatric surgery (48.8 nM) 10) .
Seminal parameters
Regarding the spermogram parameters, mixed findings were found. Although one study found a statistically significant improvement in sperm concentrations in patients with azoospermia (p = 0.02) and oligospermia (p = 0.001), with sperm finding in the ejaculate of 6 of 13 (43%) patients who initially had azoospermia7, other studies showed a reduction in total sperm count at 12 months after bariatric surgery in patients without a history of infertility (177.7 x 106 vs. 108.2 x 106 at 12 months p = 0.087), despite of improvements in the levels of total testosterone and sex hormone transporter globulin; this deterioration was seen even in patients without a history of infertility, taking into account that < 20% of the patients in this cohort had baseline oligozoospermia8. Wood et al. also evidenced that patients undergoing bariatric surgery presented a reduction in sperm concentration (110 vs. 67.3 x 106/mL p = 0.002), and in total sperm count 133.5 x 106 versus 80.7 x 106 (p = 0.002) at 6 months; even two patients with a sperm count of 0.1 and 82 million/mL presented azoospermia 6 months after being operated on11.
Discussion
Our systematic review shows the resuits of five studies from different countries, ali prospective, with a low number of patients, and with high heterogeneity.
Obesity in men has been associated with a decrease in testosterone and SHBG; in addition to an increase in estradiol, leading secondarily to hypogonadotrophic hypogonadism12,13. Male obesity-related secondary hypogonadism (MOSH) brings with it endocrine dysfunction, being reported in up to 45% in patients with moderate-severe obesity14. Regarding the compromise of the seminal parameters, these patients have a higher risk of presenting azoospermia or oligospermia, but the mechanism in which obesity affects fertility is complex and heterogeneous, both hyperinsulinemia and hyperleptinemia have a direct effect on spermatogenesis secondary to the oxidative stress and associated inflammatory state, leading to loss of DNA integrity15,16.
Campbell et al. found clear data in a meta-analysis that paternal obesity negatively affects fertility and reproductive potential17. These results have also been demonstrated in experimental studies in animals18,19. In addition, evidence has been found in both animals and humans that changes in lifestyle habits, such as physical exercise and a balanced diet, with consequent weight loss, can improve fertility20.
Sermondade et al., in a retrospective series of three cases, reported that the rapid weight loss associated with bariatric surgery was associated with significant changes in the spermogram parameters (severe oligoasthenozoospermia), which in one of the patients spontaneously improved at 2 years of the procedure and did not require assisted reproductive therapy. Our data show that bariatric surgery is associated with negative changes in the spermogram, and positive changes in sexual hormonal parameters21. It has been suggested that negative changes in the spermogram may be secondary to a catabolic state and consequently an accumulation of reactive oxygen substances at the testicular level, causing damage to both sperm and DNA22. However, more prospective studies with a greater number of patients are still needed to clarify the origin of this sperm damage, most of these studies being reports or case series6,23. Moxthe et al., carried out a systematic review of the effects of bariatric surgery on both male and female fertility, included seven studies in men, finding a significant improvement in hormonal parameters and sperm count; although the review has important weaknesses in terms of the methodology between the studies, which do not specify posible confounding variables24. Samavat et al. found an improvement in seminal count, motility, and ejaculate.
Samavat et al. found an improvement in seminal count, motility, and ejaculate after bariatric surgery, and showed a decrease in sperm DNA fragmentation25. On the contrary, Legro et al. found no improvement in the seminal parameters of patients taken to gastric bypass26. Some reports have shown a negative effect on semen quality secondary to the nutritional deficit associated with surgical procedures related to a catabolic state (extrapolated data from very weak evidence, which require randomized studies to be corroborated)21,23,27.
Our study has certain limitations, starting with the low number of studies found to carry out the systematic review, the high degree of heterogeneity that existed in the studies for most of the measures, which reduced the comparison of the different hormonal and sperm parameters.
Conclusions
Our systematic review shows the positive results of bariatric surgery on sexual hormonal parameters in men, with an increase in total testosterone levels. No positivity was found in post-surgical sperm changes. More prospective and randomized studies are required, hopefully of Latin American population, which can help confirm this association to draw more conclusions in the future.