Introduction
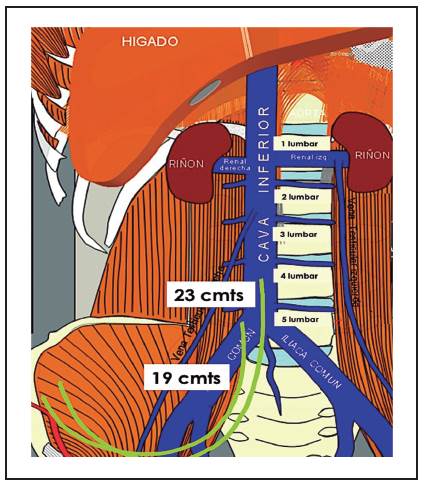
Native arteriovenous fistulae are the best option for hemodialysis patients, the second one is the arteriovenous synthetic grafts[1,2]. However, in our country, 70% of incident patients to hemodialysis start therapy with a non-programed procedure[3]. Furthermore, the main etiologies of CKD are diabetes and hypertension, diseases that are associated to poor quality vessels and with poorer results in the construction and performance of the native access. In the superior thorax, different routes are depicted to use bilumen catheters. Internal jugular vein is the most frequently used[4], but innominate[5], axillary[6,7], and superior cava vein- are also other alternatives, with a last resort being implantation in the right atrium[9]. If the superior thorax vessels are exhausted the next alternatives for vascular access are in the lower hemithorax[10]. The femoral vein is a very good option, and is used often for transitory catheters, there are few papers related with long term results of this vascular access, and with significant number of patients in dialysis with long term, tunneled, catheters[11]. The general concept is better outcomes and better flux can be obtained with catheters which tip are in vessels with bigger diameter, thus with longer times, better dialysis dose, and less infectious and thrombotic complications. For Internal jugular vein catheters, the KDIGO guidelines establish the right atrium as the right position, this placement is achieved with 15 to 20 cm catheters, for the femoral accesses the right position is the inferior cava vein, this is achieved with 19 to 24 cm catheters[12]. In this paper, we describe our experience with a significant number of cases with two different lengths of tunneled catheters placed in the femoral vein, with different positioning of the tip, and we report the long term outcomes and complications.
Materials and methods
Nineteen CKD E5D patients, over eighteen years, were included, with 30 procedures of implantation, all of them needed a vascular access for chronic hemodialysis, and in all of them, another possible vascular catheter or arterial-venous fistulae, was excluded, furthermore the patients declined to begin peritoneal dialysis.
Demographic variables were gender; age, previous time in hemodialysis, number of previous catheters, type (no tunneled vs. tunneled) and location.
All the patients signed informed consent for the procedures.
The implantation procedures were performed in the procedure room of dialysis facilities by two experienced nephrologists in central venous catheters (CVC) implantation. All the procedures were made with B mode ultrasonography guide to locate the femoral vein and subsequent puncture of them. The procedures were made with local anesthesia, blood pressure monitoring and pulse oximetry.
For commodity of both, right handed, nephrologists, the right femoral vein was preferred first. If the ultrasonographic evaluation showed a bigger diameter, or if the metallic guide wire didn't progress easily inside the right femoral vein, the left vein was used as second option.
The procedures were done under aseptic conditions and with local anesthesia in the skin a tissue over the territory of the vascular-nervous complex femoral. The femoral vein was punctured, guide wire was passed and left in the vessel lumen and the needle was removed. Then we applied local anesthesia in the supra-inguinal region, in a horizontal trajectory of 2 cm, and about 10 cm distant of the vein puncture site. Then we applied local anesthesia along the trajectory from de supra-inguinal region until venous puncture site. With a scalpel, an incision was made in the supra-inguinal area and a subcutaneous tunnel was made advancing a tunneler from the incision to the exit site of wire guide, the catheter was introduced in the tunnel joined to the tunneler. Over the guide wire the vein was dilated with 12 French and 14 French dilators, then a 16 French Valved Pull-Apart Sheath/Dilator was advanced to the vein, the dilator was removed and the flexible catheter was advanced at time the sheath was removed. Patency was verified, the incisions were sutured and the catheter was fixed to the skin of the anterior wall of the abdomen (figure 1,2).

Figure 1 19 cm (from cuff to tip) length femoral catheter, the tip location is mainly in the iliac vein.
After the implantation, a plain of abdomen was obtained to confirm the tip positioning (figure 1,2)
Complications during the procedure and 48 hours after were recorded (arterial puncture, lacerations to the vessels, retroperitoneal bleeding, hematoma). Long term complications were also recorded: venous thrombosis, kinking, displacement, extrusion, exit site infection, catheter related sepsis or bacteremia, pulmonary embolism.
Also, the operational time and the removing cause: malfunctioning, catheter related sepsis, exit site infection, peritoneal dialysis therapy change, renal transplantation, catheter functioning death.
The procedure was declared successful if the blood flow (Qb) was over 200 ml/min.
Patients were allocated in two groups: the first (G1) had 8 patients which catheter were implanted between February 2009 to February 2014, in these days we only had 19 cm (length from the cuff to the tip) catheters, the second group (G2) had 11 patients which catheters were implanted from march 2011 to September 2017, in this period we had similar catheters but with 23 cm length (from cuff to tip).
To evaluate if the differences between both groups were statistically significant, the distribution probe "F" with the respective "p" value (the value for "p" was significant if inferior to 0.05) were used.
Results
During 103 months (from February 2009 to September 2017), 30 femoral tunneled catheters were implanted in 19 patients; 15 each group, mean age was 56.3 years. Thirteen (68.4%) were men.
The total number of previously implanted catheters was 63; 28 in G1 (mean 1.9/patient), and 35 in G2 (mean 2, 4/patient).
Previous sites for G1 were: jugular 17, axillary 3, innominate 1, no tunneled femoral 7; for G2 there were jugular 23, axillary 3, innominate 0, no tunneled femoral 10.
The mean functioning time for G1 was 132 +/- 164 days, and 234 +/- 172 days, the time was superior for G2, but was not statistically significant between groups (table 1).
The retirement causes for G1 were: malfunctioning by cloths 8(53%), change of access (arteriovenous fistula) 2, Renal transplantation 1, change to peritoneal dialysis (PD) 1, catheter related sepsis 1 and death 2; for G2 were: malfunctioning by cloths 6(40%), change of access (arteriovenous fistula) 2, renal transplantation 0, change to PD 3, catheter related sepsis 0, death 2, active at cutting point 2. The percentage difference of retirement for malfunctioning was not statistically significant (40 Vs. 53%).
Regarding the complications, any group had major bleeding, both during insertion or retirement. The procedure of retirement was performed for the same nephrologists, with local anesthesia in minor procedures room.
The radiographic control showed the 19 cm catheters tip between S1 and L5 (approximately iliac vein bed), meanwhile the 23 cm tip catheters was located between L3 and L4, area of the inferior cava vein (figures 1,2).
There were no differences for numbers of previous catheters, hemodialysis time and functioning time between both groups, the table 2 shows the 'F' Value, with the respective "p" value, all superior to cutting point (table 2).
Discussion
Femoral veins tunneled catheters are a valuable option in patients with "classic" routes exhausted.
The international consensus establishes the catheters tip ideally located in big diameter vessels to obtain better Qb (12), which means longer catheters. However, the fluid physics is complex, the blood flux decreases with de catheter length and is better as the diameter increases. Furthermore, the flux change to turbulent instead of laminar with the curvatures that are frequent in tunneled femoral catheters, with turbulent flux the velocity is low and the environment is prone to thrombosis[13]. For femoral catheters is recommended the tip was located in the inferior cava vein, or near to the right atrium, that requires too long catheters[12].
Often the catheter is located in inappropriate beds such as lumbar ascendant vein[14], hemyazigos accessory vein[15], is therefore important to verify the location of the tip with a simple plain radiography of the abdomen, mainly if the functioning is inadequate.
The implantation is related with complications such as Phlegmasia Cerulea Dolens[16], retroperitoneal hematoma[15,17], abdominal compartment syndrome[18], and iliac a femoral veins stenosis[19].
There are few papers related with long-term outcomes and with adequate number of tunneled catheters. Zaleski GX et al in their three-year experience with 41 catheters and with lengths from 40 to 60 cm found frequent interventions by diverse causes and an increased susceptibility to infection[20]. Chow Km et al in 14 catheters report better long-term permeability, with reasonable survival, and a lesser number of infections[21]. Falk A in his three-year experience with 86 catheters found low permeability and a significant number of complications[22]. Maya el al found in 22 patients with tunneled femoral catheters low long-term permeability vs. jugular catheters and higher risk of deep vein thrombosis, although equal risk of infections[23]. Al-Hwiesh AK in 14 patients with low follow-up time concluded these catheters are a reliable alternative for patients without any other access[24].
In our study, we observe the 19 cm length tunneled femoral catheters (from cuff to tip) the tip is located at level of iliac vein, while the 23 cm ones has the tip located in the cava vein (figure 3). Based on these observations are expected better results with de 23 cm length catheters. However, the results obtained were not different for both kinds of devices.
We can conclude that with longer femoral catheters (for example 28 to 55 cm, from cuff to tip), is likely the tip reaches major diameter venous beds, which allows better Qb, lesser possibility of thrombosis and better dose of dialysis.