Introduction
Obscure gastrointestinal bleeding, defined as bleeding without identification of the source, accounts for 10% of all cases of gastrointestinal hemorrhage. Bleeding from the small intestine is the leading cause of obscure bleeding, comprising 5%-10% of all cases of gastrointestinal tract bleeding1, which includes the region between the ampulla of Vater and the ileocecal valve. Among the various lesions, vascular causes represent 70%-80% of cases, followed by tumors in 5%-10%2. Small intestinal hemangiomas are considered rare, accounting for 7%-10% of all benign small bowel tumors. The most common clinical manifestations include bleeding, abdominal pain, obstruction, intussusception, or perforation3. Bleeding is predominantly chronic, with secondary iron-deficiency anemia as the main consequence4. The use of capsule endoscopy and device-assisted enteroscopy in recent years has enabled complete evaluation of the small intestine and diagnosis of such lesions. The first-line treatment is surgical resection. We present the case of a young patient experiencing massive gastrointestinal bleeding due to a jejunal capillary hemangioma, which was diagnosed by intraoperative enteroscopy and successfully managed with surgical resection.
Case Presentation
A 21-year-old female patient with no known medical history presented with an acute episode of rectal bleeding, accompanied by abdominal pain, nausea, and general discomfort. Upon admission to a medical center, persistent bleeding was documented, resulting in anemia and necessitating the transfusion of four units of packed red blood cells and three units of plasma. An esophagogastroduodenoscopy was performed, revealing erythematous antral gastritis, and a total colonoscopy showed grade I internal hemorrhoids with no signs of active bleeding. However, clinically, the patient continued to experience two to three episodes of melena daily.
In preparation for a small intestine bleeding study, capsule endoscopy was planned. However, during her stay, she developed hemodynamic instability with tachycardia and hypotension, requiring stabilization and subsequent referral for angiography and embolization to control the bleeding. Upon arrival at the institution, she was hemodynamically stable and did not require vasopressor support. A second esophagogastroduodenoscopy was conducted, showing chronic erythematous gastritis and antral follicular gastritis. During follow-up, the patient once again exhibited signs of hemorrhagic shock, with ongoing profuse melena and significant anemia within less than 24 hours, with hemoglobin levels dropping from 9.7 g/dL to 3.9 g/dL. Consequently, an abdominal aortogram with selective mesenteric vessel study was performed, which was reported as normal for her age (Figure 1).
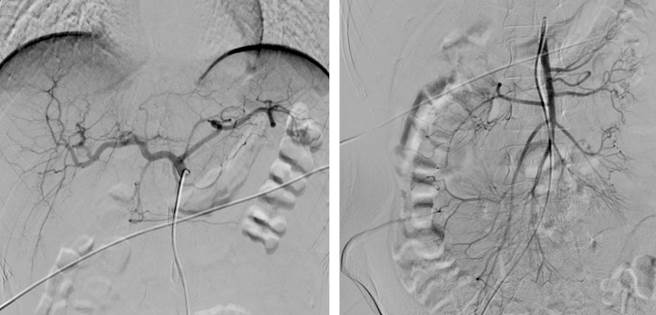
Source: Author’s File.
Figure 1 Abdominal aortogram and selective mesenteric vessel study within normal limits for age.
Due to the patient’s clinical instability and the negative angiographic study, a multidisciplinary team decided to proceed with intraoperative enteroscopy. An open laparotomy was performed, identifying the ligament of Treitz, at which point an enterotomy was made, and a colonoscope was introduced. In the proximal jejunum, a pedunculated polypoid lesion was identified, measuring approximately 15 mm at the head and 10 mm at the stalk, with active bleeding observed (Figure 2). A hemostatic clip was placed to partially control the bleeding and facilitate the surgical resection of a 30 cm segment of the jejunum with a side-to-side anastomosis.
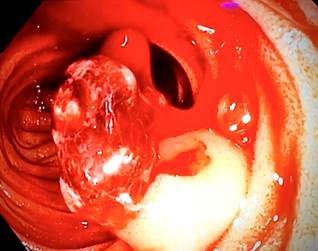
Source: Author’s File.
Figure 2 Intraoperative enteroscopy. Polypoid lesion in the jejunum with active bleeding.
Pathology examination reported a well-circumscribed benign mesenchymal tumor located in the submucosa and muscularis propria, consisting of thin-walled vascular channels without atypia or mitosis, filled with abundant blood, consistent with an ulcerated capillary hemangioma (Figures 3 and 4). The patient showed a favorable clinical course, with no new bleeding episodes, improved hemoglobin levels, and good tolerance to oral intake, allowing for discharge. She remains asymptomatic in outpatient follow-up.
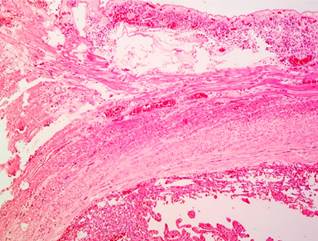
Source: Author’s File.
Figure 3 Capillary hemangioma of the jejunum. Hematoxylin-eosin stain, 40x. Involvement of the submucosal and muscularis propria layers.
Discussion
Hemangiomas account for 0.05% of all gastrointestinal tract neoplasms. They can be classified by the type of vessels involved as capillary, cavernous, or mixed types and are composed of small terminal blood vessels. Their presence in the small intestine is exceedingly rare, with only a few cases reported to date4. Although considered a benign condition, hemangiomas have the potential to cause complications, primarily chronic bleeding over time, which can lead to iron-deficiency anemia. While they can be successfully treated with surgical resection, their rarity in younger patients and their anatomical location may prevent them from being considered in differential diagnoses. Furthermore, routine examinations like computed tomography, magnetic resonance imaging, and colonoscopy often face limitations in identifying these lesions. Therefore, diagnostic studies for the small intestine, such as capsule endoscopy or double-balloon enteroscopy, have become the best tools for preoperative evaluation of lesions in the ileum and jejunum in hemodynamically stable patients5.
In this case, due to the patient’s hemodynamic instability, which necessitated transfusion support and vasopressor use, an abdominal angiography was initially performed but yielded negative results. Consequently, intraoperative enteroscopy was ordered as a last resort to determine the bleeding source and achieve prompt control, in line with current recommendations for managing small intestine bleeding1,6,7. Subsequently, the standard treatment of surgical resection with side-to-side anastomosis was carried out, resulting in a satisfactory postoperative course.
This case highlights the significance of intraoperative enteroscopy as a fundamental tool in managing small intestine bleeding in patients with persistent hemodynamic instability, even after a negative abdominal vessel angiography. In such cases, it should not be deferred or replaced by procedures like capsule endoscopy, as intraoperative enteroscopy not only allows diagnosis but also facilitates immediate treatment within the same procedure. In this case, intraoperative enteroscopy was preferred over capsule endoscopy due to the latter’s lower sensitivity for detecting arteriovenous malformations (as low as 50%), mainly because it lacks insufflation and suction capabilities, which hinders the inspection of folds and lengthens the procedure time and result interpretation. Additionally, arteriovenous malformations can sometimes be detected through transillumination of the external surface of the intestinal wall, which is only feasible with intraoperative enteroscopy8,9.
The histopathological study confirmed the diagnosis of capillary hemangioma of the jejunum, and this histological subtype is also considered particularly rare. In a study of 37 reported cases from 2000 to 2018, only three exhibited the capillary subtype, while the rest showed the cavernous subtype3. Additionally, diagnosis in these cases was made preoperatively using capsule endoscopy or balloon-assisted enteroscopy in hemodynamically stable patients. The most common treatment for these hemangiomas is surgical resection. However, in recent years, less invasive endoscopic therapies, such as polidocanol sclerotherapy, have shown promising results, along with other therapies like argon plasma coagulation and endoscopic mucosal resection. Nevertheless, special caution is required to prevent complications such as perforation, arterial aspiration, and puncture-related issues, especially in cases of transmural hemangiomas, as in this instance, where endoscopic therapy alone might not suffice for complete treatment of the lesion10,11.
Conclusion
We report the case of a young adult patient with a solitary capillary hemangioma in the jejunum that caused acute bleeding, leading to hemorrhagic shock and necessitating intraoperative enteroscopy and jejunal surgical resection. These types of lesions pose diagnostic challenges with conventional methods like computed tomography, magnetic resonance imaging, or colonoscopy. Although capsule endoscopy and balloon enteroscopy can aid in characterizing them, in patients with persistent or recurrent hemodynamic instability, as seen in this case, intraoperative enteroscopy should be the procedure of choice, as it allows for lesion localization and urgent management. Finally, although these lesions are rare, they should be considered in the differential diagnosis of gastrointestinal bleeding originating in the small intestine, especially in young patients with massive bleeding episodes.











 text in
text in 




